Avicenna Journal of Clinical Microbiology and Infection. 8(2):81-83.
doi: 10.34172/ajcmi.2021.14
Letter
What is the Relationship between Helicobacter pylori Infection and Gastroesophageal Reflux Disease (GERD)? A Comprehensive Analysis on Iranian Population
Amir Yousefi 1, Masoud Keikha 1, * 
Author information:
1Department of Microbiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
*
Corresponding author: Masoud Keikha; PhD, Department of Microbiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. Email:
masoud.keykha90@gmail.com
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Dear Editor,
Helicobacter pylori is a gram-negative, microaerophilic, and rod-shaped bacterium, which is colonized in human gastric-submucosa of approximately 4-4.5 billion people throughout the worldwide (1-2). The bacterium can cause chronic gastritis and increase the risk of developing gastric adenocarcinoma by 10 times, as well as peptic ulcer disease (3). According to the literature, H. pylori infection has clinical benefits in prevention of several diseases such as autoimmune diseases, asthma, celiac, and irritable bowel syndrome (4-7). There are several conflicting reports on the probable association between H. pylori infection and gastroesophageal reflux disease (GERD) (8-9).
GERD is a digestive complication in which acidic stomach juices revert up from the stomach into the esophagus and acidic pH causes tissue damages (10). The prevalence of GERD was lower in countries with high burden of H. pylori infection. H. pylori infection has a protective role in regression of GERD, though the main mechanism is still unclear (11,12). For the first time, we evaluated the impact of H. pylori infection in risk of GERD in an Iranian population with comprehensive statistical analysis.
We performed a systematic literature search using search terms including ‘H. pylori’, ‘Helicobacter pylori’, ‘Gastro-oesophageal reflux diseases’, ‘Reflux oesophagitis’, and ‘Iran’ in several international databases including Medline, Scopus, Embase, and Google Scholar and retrieved all the related articles. Then, the title, abstract, and full-text of relevant reports were screened, and all case-control studies on an Iranian population were included in the study. The required data such as first author, publication year, city, age, gender distribution, number of case and control in each individual studies, frequency of H. pylori infection in each groups, diagnostic methods, and reference numbers were extracted and summarized in the Table 1.
Table 1.
Characteristics of included studies
|
First author
|
Year of Publication
|
Area
|
Age (y)
|
Gender (F/M)
|
Case
(n)
|
Control (n)
|
No. of
H
. pylori Infection |
Diagnostic method
|
Ref.
|
|
Case
|
Control
|
Case
|
Control
|
Case
|
Control
|
| Zali |
2003 |
Tehran |
49 |
49 |
NA |
NA |
51 |
51 |
23 |
22 |
UBT |
13 |
| Siadati |
2014 |
Babol |
49 |
43 |
244/330 |
191/155 |
574 |
346 |
189 |
110 |
Culture |
14 |
| Abdollahi |
2011 |
Tehran |
5.3 |
4.8 |
29/30 |
105/99 |
59 |
204 |
13 |
70 |
UBT |
15 |
| Somi |
2008 |
Tabriz |
43.1 |
42.7 |
45/47 |
47/46 |
92 |
93 |
75 |
81 |
UBT |
16 |
| Khoshbaten |
2013 |
Tehran |
45.7 |
47.2 |
40/70 |
40/70 |
55 |
55 |
25 |
32 |
Culture |
17 |
| Shavalipour |
2017 |
Tehran |
45.7 |
41.2 |
29/21 |
27/23 |
50 |
50 |
27 |
31 |
Culture |
18 |
| Nobakht |
2016 |
Tehran |
58.3 |
58.3 |
NA |
NA |
367 |
367 |
102 |
216 |
Culture |
19 |
| Rasmi |
2009 |
Urmia |
26.4 |
25.9 |
38/47 |
45/24 |
85 |
69 |
60 |
56 |
ELISA |
20 |
| Mirzaei |
2007 |
Rafsanjan |
37.4 |
37.6 |
14/15 |
41/40 |
19 |
81 |
3 |
31 |
UBT |
21 |
| Masjedizadeh |
2006 |
Tehran |
54.1 |
52.2 |
20/31 |
29/20 |
51 |
49 |
45 |
38 |
UBT |
22 |
We pooled the data to investigate the probable association between H. pylori infection and GERD by odds ratio (OR) corresponding to 95% confidence intervals (CIs). Furthermore, the association between cagA positive H. pylori strains and GERD risk was also measured in the current analysis. Heterogeneity was dignified by I2 index and Cochrane P value test; the random-effects models were applied for the case of significant heterogeneity. Otherwise, the fixed-effects models were used in lack of heterogeneity cases. Moreover, the publication bias was also determined by Begg’s and Egger’s P value test (23).
In the current quantitative analysis, we collected 107 relevant articles in the primary literature search. After reviewing the full-texts, 10 case-control studies were included. These studies were performed between 2003 and 2017 in various cities including Tehran (n=6), Tabriz (n=1), Babol (n=1), Urmia (n=1), and Rafsanjan (n=1). In the eligible studies, we pooled the data of 2,768 human subjects. There were 1,403 cases (mean age: 41.4 years, female: 37.2%, male: 62.8% ) and 1,365 controls (mean age: 40.1 years, female: 39.9%, male: 60.1%). The H. pylori infection rate was 38.6% in cases and 49% in healthy subjects. In these studies, the H. pylori infection was diagnosed based on the conventional microbiology methods, urease breath test, and ELISA. Our results indicated a significant inverse association between H. pylori infection and GERD in an Iranian case (OR: 0.6; 95% CI: 0.50-0.71; P = 0.001; I2: 81.93; Q-Value: 49.82; P = 0.001; Egger’s P =0.69; Begg’s P= 0.72). Interestingly, infection with cagA expressing H. pylori strains can reduced the risk of susceptibility to GERD in the patients by 0.5 fold (OR: 0.54; 95% CI: 0.34-0.86; P = 0.009; I2: 78.2; Q-Value: 9.1; P = 0.01; Egger’s P = 0.53; Begg’s P = 0.5). Therefore, the summary OR showed that H. pylori infection can have an inverse association with developing GERD in an Iranian population (Figure 1).
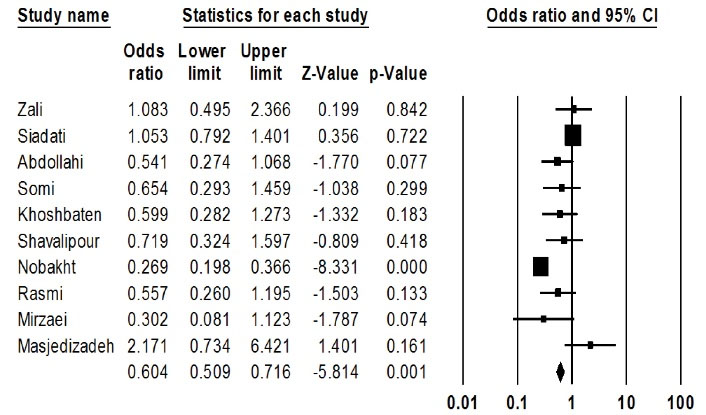
Figure 1.
The Odds Ratio at 95% Confidence Interval for the Assessment of Association between H. Pylori Infection and GERD in an Iranian Population.
.
The Odds Ratio at 95% Confidence Interval for the Assessment of Association between H. Pylori Infection and GERD in an Iranian Population.
The GERD is one of the common gastrointestinal disorders worldwide. It has been estimated that approximately more than 40% of people have experienced GERD in their lives (24). In recent years, the impact of the H. pylori infection in GERD has gain attention. However, there are conflicting results about the association between the bacterium and GERD (25,26). Therefore, it is necessary to conduct a larger experiment to determine the effect of H. pylori infection in GERD immune-pathogenesis. In the current report, we pooled all available data regarding the evaluation of H. pylori in GERD in an Iranian population. The results suggested that H. pylori infection particularly cagA positive strain can hamper the risk of developing GERD in an Iranian population. Our results confirmed the findings of a meta-analysis by Cremonini et al, indicating a significant association between the absence of H. pylori infection and GERD symptoms (27). Overall, it can be considered that H. pylori infection has an inverse association with developing GERD symptoms.
Conflict of Interests
None.
References
- Kusters JG, van Vliet AH, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev 2006; 19(3):449-90. doi: 10.1128/cmr.00054-05 [Crossref] [ Google Scholar]
- Yousefi B, Mohammadlou M, Abdollahi M, Salek Farrokhi A, Karbalaei M, Keikha M. Epigenetic changes in gastric cancer induction by Helicobacter pylori. J Cell Physiol 2019; 234(12):21770-84. doi: 10.1002/jcp.28925 [Crossref] [ Google Scholar]
- Wroblewski LE, Peek RM Jr, Wilson KT. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbiol Rev 2010; 23(4):713-39. doi: 10.1128/cmr.00011-10 [Crossref] [ Google Scholar]
- Youssefi M, Tafaghodi M, Farsiani H, Ghazvini K, Keikha M. Helicobacter pylori infection and autoimmune diseases; Is there an association with systemic lupus erythematosus, rheumatoid arthritis, autoimmune atrophy gastritis and autoimmune pancreatitis? a systematic review and meta-analysis study. J Microbiol Immunol Infect 2020. doi: 10.1016/j.jmii.2020.08.011 [Crossref]
- Arnold IC, Dehzad N, Reuter S, Martin H, Becher B, Taube C. Helicobacter pylori infection prevents allergic asthma in mouse models through the induction of regulatory T cells. J Clin Invest 2011; 121(8):3088-93. doi: 10.1172/jci45041 [Crossref] [ Google Scholar]
- Amlashi FI, Norouzi Z, Sohrabi A, Shirzad-Aski H, Norouzi A, Ashkbari A, et al. A systematic review and meta-analysis for association of Helicobacter pylori colonization and celiac disease. bioRxiv. 2020. 10.1101/2020.10.12.335836
- Wu XW, Ji HZ, Yang MF, Wu L, Wang FY. Helicobacter pylori infection and inflammatory bowel disease in Asians: a meta-analysis. World J Gastroenterol 2015; 21(15):4750-6. doi: 10.3748/wjg.v21.i15.4750 [Crossref] [ Google Scholar]
- Kim BC, Yoon YH, Jyung HS, Chung JB, Chon CY, Lee SI. [Clinical characteristics of gastroesophageal reflux diseases and association with Helicobacter pylori infection]. Korean J Gastroenterol 2006; 47(5):363-9. [ Google Scholar]
- Abdul-Razzak KK, Bani-Hani KE. Increased prevalence of Helicobacter pylori infection in gastric cardia of patients with reflux esophagitis: a study from Jordan. J Dig Dis 2007; 8(4):203-6. doi: 10.1111/j.1751-2980.2007.00306.x [Crossref] [ Google Scholar]
- Jonaitis LV, Kiudelis G, Kupcinskas L. Characteristics of patients with erosive and nonerosive GERD in high-Helicobacter-pylori prevalence region. Dis Esophagus 2004; 17(3):223-7. doi: 10.1111/j.1442-2050.2004.00412.x [Crossref] [ Google Scholar]
- Haruma K. Review article: influence of Helicobacter pylori on gastro-oesophageal reflux disease in Japan. Aliment Pharmacol Ther 2004; 20 Suppl 8:40-4. doi: 10.1111/j.1365-2036.2004.02228.x [Crossref] [ Google Scholar]
- Malfertheiner P, Peitz U. The interplay between Helicobacter pylori, gastro-oesophageal reflux disease, and intestinal metaplasia. Gut 2005; 54 Suppl 1:i13-20. doi: 10.1136/gut.2004.041533 [Crossref] [ Google Scholar]
- Zali MR, Masjedizadeh A, Moezardalan K, Samie S. Atrophic gastritis and Helicobacter pylori infection in patients with reflux esophagitis: a case-control study. Am J Gastroenterol 2003; 98(s9):S44. doi: 10.1111/j.1572-0241.2003.07862.x [Crossref] [ Google Scholar]
- Siadati S, Fotok-Kiai SZ, Shokri-Shirvani J. Association of Helicobacter pylori infection and erosive reflux esophagitis in patients with GERD. J Babol Univ Med Sci 2014; 16(4):7-13. [ Google Scholar]
- Abdollahi A, Morteza A, Khalilzadeh O, Zandieh A, Asgarshirazi M. The role of Helicobacter pylori infection in gastro-oesophageal reflux in Iranian children. Ann Trop Paediatr 2011; 31(1):53-7. doi: 10.1179/1465328110y.0000000004 [Crossref] [ Google Scholar]
- Somi MH, Fattahi E, Fouladi RF, Karimi M, Bonyadi R, Baballou Z. An inverse relation between CagA+ strains of Helicobacter pylori infection and risk of erosive GERD. Saudi Med J 2008; 29(3):393-6. [ Google Scholar]
- Khoshbaten M, Baghaei K, Bafandeh Y, Saeidi GR, Gachkar L, Al Dulaimi D. The role of Helicobacter pylori and CagA in response to treatment in Iranian Gastroesophageal Reflux Diseases patients. Gastroenterol Hepatol Bed Bench 2013; 6(Suppl 1):S93-8. [ Google Scholar]
- Shavalipour A, Malekpour H, Dabiri H, Kazemian H, Zojaji H, Bahroudi M. Prevalence of cytotoxin-associated genes of Helicobacter pylori among Iranian GERD patients. Gastroenterol Hepatol Bed Bench 2017; 10(3):178-83. [ Google Scholar]
- Nobakht H, Boghratian A, Sohrabi M, Panahian M, Rakhshani N, Nikkhah M. Association between pattern of gastritis and gastroesophageal reflux disease in patients with Helicobacter pylori infection. Middle East J Dig Dis 2016; 8(3):206-11. doi: 10.15171/mejdd.2016.33 [Crossref] [ Google Scholar]
- Rasmi Y, Sadreddini M, Shahsavari Z, Raeisi S. Prevalence of Helicobacter pylori and cytotoxin-associated gene A in Iranian patients with non-erosive and erosive reflux disease. Indian J Med Sci 2009; 63(9):402-7. doi: 10.4103/0019-5359.56113 [Crossref] [ Google Scholar]
- Seyedmirzaei SM, Mikaeili J, Sajadi SAR. Induction of esophagal reflux after eradication of Helicobacter pylori. J Rafsanjan Univ Med Sci 2007; 6(3):187-92. [ Google Scholar]
- Masjedizadeh R, Hajiani E, Moezardalan K, Samie S, Ehsani-Ardakani MJ, Daneshmand A. H pylori infection and reflux oesophagitis: a case-control study. World J Gastroenterol 2006; 12(35):5658-62. doi: 10.3748/wjg.v12.i35.5658 [Crossref] [ Google Scholar]
- Karbalaei M, Keikha M. Potential association between the hopQ alleles of Helicobacter pylori and gastrointestinal diseases: a systematic review and meta-analysis. Meta Gene 2020; 26:100816. doi: 10.1016/j.mgene.2020.100816 [Crossref] [ Google Scholar]
- Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet 1951; 92(4):419-31. [ Google Scholar]
- Grande M, Cadeddu F, Villa M, Attinà GM, Muzi MG, Nigro C. Helicobacter pylori and gastroesophageal reflux disease. World J Surg Oncol 2008; 6:74. doi: 10.1186/1477-7819-6-74 [Crossref] [ Google Scholar]
- Moon A, Solomon A, Beneck D, Cunningham-Rundles S. Positive association between Helicobacter pylori and gastroesophageal reflux disease in children. J Pediatr Gastroenterol Nutr 2009; 49(3):283-8. doi: 10.1097/MPG.0b013e31818eb8de [Crossref] [ Google Scholar]
- Cremonini F, Di Caro S, Delgado-Aros S, Sepulveda A, Gasbarrini G, Gasbarrini A. Meta-analysis: the relationship between Helicobacter pylori infection and gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2003; 18(3):279-89. doi: 10.1046/j.1365-2036.2003.01665.x [Crossref] [ Google Scholar]