Avicenna Journal of Clinical Microbiology and Infection. 8(2):39-44.
doi: 10.34172/ajcmi.2021.08
Original Article
Clinical and Para-clinical Features of Brucellosis With and Without Spondylodiscitis
Fariba Keramat 1  , Seyyed Hamid Hashemi 1, *
, Seyyed Hamid Hashemi 1, *  , Farzaneh Esna-ashari 2, Kaveh Kaseb 3
, Farzaneh Esna-ashari 2, Kaveh Kaseb 3
Author information:
1Brucellosis Research Center, Department of Infectious Diseases, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Community of Medicine, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
3General Practitioner, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
*
Corresponding author: Seyyed Hamid Hashemi, Brucellosis Research Center, Sina Hospital, MirzadehEshghi Street, Hamadan, 65168, Iran Tel: +98 918 1113258. Email:
shahashemi@yahoo.com
Abstract
Background: Brucellosis is a common zoonotic disease with protean clinical manifestations. Osteoarticular involvement is the most common complication of the disease. This study aimed to compare the clinical and para-clinical manifestations of brucellosis among the patients with and without spondylodiscitis.
Methods: In this comparative and cross-sectional study, 135 patients having brucellosis with and without spondylodiscitis and admitted to Sina hospital in Hamadan, Iran from March 2009 to March 2014 were included. Clinical and para-clinical data of the patients were obtained from their medical records in the hospital based on a designed checklist.
Results: Thirty-five patients having brucellar spondylodiscitis (BS) with the mean age of 55.60±14.31 years, and 100 patients having brucellosis without BS with the mean age of 43.27±18.35 years were examined. A significant difference was found between the mean age of the patients with spondylodiscitis and that of those without spondylodiscitis (P<0.001). All patients with spondylodiscitis complained of back pain and vertebral tenderness, while 60% of the patients without BS suffered from back pain but experienced no vertebral tenderness (P=0.003). The most common vertebral involvement in spinal MRI of the patients with BS was L4-L5 (45.7%). Patients with spondylodiscitis had more increased ESR and CRP than those without spondylodiscitis (P<0.001).
Conclusion: It is recommended that Brucellar spondylodiscitis be considered in the differential diagnosis of the patients with prolonged fever, back pain, and vertebrae tenderness in the endemic areas.
Keywords: Brucellosis, Spondylodiscitis, Clinical manifestations
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Introduction
Brucellosis is the most common zoonotic disease caused by Brucella spp. which is transmitted from infected animals to humans through various ways such as consumption of contaminated dairy products or direct contact with animals.It is a major public health issue throughout the world.Annually, 500 000 cases with brucellosis are reported to the World Health Organization (WHO), most of whom are from the developing countries (1).The disease is an endemic in Iran and, according to the annual report of Center for Disease Control of Ministry of Health and Medical Education in Iran, the incidence rates of brucellosis were 81.4 and 90.7 per 100 000 people in Hamadan, west of Iran in 2013 and 2014, respectively (2). The most common local involvement of the disease is in the musculoskeletal system (1,3,4). According to the results from several studies, the local involvements of spinal vertebra, clinical manifestations, as well as the frequency of paraspinal and epidural abscesses differ (5-10). Since Brucellar Spondylodiscitis (BS) is a serious and destroying complication, early diagnosis and proper treatment of brucellosis may prove useful in preventing the disabilities caused by it (7-11).
This study, therefore, aimed to compare clinical and para-clinical manifestations of brucellosis between the patients with spondylodiscitis and those without it in order for developing a method of diagnosis and treatment for skeletal complications of brucellosis.
Materials and Methods
Study Design
In this comparative cross-sectional study conducted in Hamadan, Iran, all patients having brucellosis with and without spondylodiscitis and having been admitted in Sina hospital from March 2009 to March 2014 were included. It is noteworthy that Sina hospital was the main referral center for infectious diseases in Hamadan province located in the west of Iran.
Exclusion criteria were as follow: patients with pyogenic, tuberculous, or ankylosing spondylitis; those with endocarditis, hepatitis, epididymo-orchitis or neurobrucellosis; and those aged under 15.
Diagnosis of Brucellosis
Brucellosis was diagnosed based on clinical presentations compatible with brucellosis in the presence of significant titers of specific antibodies (standard tube agglutination ≥ 1/160, Coombs test ≥ 1/160, 2-mercaptoetanol ≥1/80) and/or a positive blood culture in Castaneda’s biphasic medium.Standard tube agglutination tests and 2ME solution were obtained from Pasteur Institute of Iran.
Spondylodiscitis was defined as inflammation of vertebral body and intervertebral disc confirmed by magnetic resonance imaging (MRI).
Study Populations
A total of 135 patients with brucellosis were included in the present study. Out of 135 patients, 25.9% of them had BS and 74.1% of them had brucellosis without BS.
Spinal MRI was carried out for all patients with skeletal back pain. A detailed medical history including the patients’ clinical and para-clinical information was extracted from their medical records. The data was recorded in the designed checklists. All demographic characteristics such as age, sex, region of living, potential risk factors, occupation, clinical manifestations, laboratory findings, and imaging reports (MRI) of the patients with brucellosis were recorded in the checklists.
Statistical Analysis
The collected data were analyzed using SPSS statistical package, version 16. Mann–Whitney U test and t test were used for obtaining quantitative variables, and chi-square test was applied for obtaining qualitative variables. Logistic regression analysis was performed to determine the risks of spondylodiscitis according to the presence of each variable. Multivariate logistic regression analysis was adopted to identify independent risk factors for spondylodiscitis. Differences with a P value of < 0.05 were considered statistically significant.
Results
Thirty-five patients (25 males and 10 females) having BS with the mean age of 55.60 ± 14.31 years (range: 32-81 years) and 100 patients (67 males and 33 females) having brucellosis without BS with the mean age of 43.27 ± 18.35 years (range: 16-85 years) were studied. There was significant difference between the patients with and without spondylodiscitis (P <0.001) in terms of age. As shown in Table 1, 71.4% of the patients with BS were males and 67% of them without spondylodiscitis were also male. No significant difference was observed between two groups in terms of sex, neighborhood, and occupation. Moreover, there were no statistically significant difference between two groups regarding the history of contact with domestic animals, consumption of unpasteurized dairy products, and previous brucellosis and brucellosis in family members (Table 1).
Table 1.
Demographic Characteristics of the Patients With and Without Brucellar Spondylodiscitis
|
Variable
|
Brucellosis patients
|
P-
value
|
With spondylodiscitis
n=35(25.9%)
|
Without spondylodiscitis
n=100 (74.1%)
|
| Mean age (yrs)±SD |
55.60±14.31
(range= 32-81yrs) |
43.27±18.35
(range=16-85yrs) |
< 0.001 |
Sex
Male/Female |
25/10 |
67/33 |
0.732 |
Neighborhoods
Rural
Urban |
25
10 |
70
30 |
0.873 |
Occupation
Stockbreeder
Farmer
others |
5
10
20 |
14
29
57 |
0.998 |
Contact with domestic animals
Yes
No |
21
14 |
47
53 |
0.186 |
Consumption of unpasteurized dairy products
Yes
No |
35
0 |
100
0 |
- |
History of previous brucellosis
Yes
No |
16
19 |
29
71 |
0.071 |
History of brucellosis in family members
Yes
No |
15
20 |
37
63 |
0.54 |
The mean duration of symptoms before the diagnosis in patients with and without spondylodiscitis were approximately 73.17 ± 68.00 and 64.70 ± 128.65 days, respectively. There was no statistically significant difference between two groups in this regard.
The most common clinical manifestations in the patients with spondylodiscitis were back pain (100%), vertebral tenderness (100%), fever (85.7%), and weight loss (37.1%). As shown in Table 2, patients with spondylodiscitis had significantly higher rates of back pain, vertebral tenderness, and weight loss compared to those without spondylodiscitis.
Table 2.
Comparison of Clinical Manifestations Between Brucellosis Patients With and Without Spondylodiscitis
|
|
With spondylitis
(n=35)
|
Without spondylitis
(n=100)
|
|
| Back pain |
35(100%) |
60(60%) |
< 0.001 |
| Fever (symptom) |
30(85.7%) |
76(76%) |
> 0.05 |
| Chillness |
28(80%) |
74(74%) |
> 0.05 |
| Malaise |
18(54.1%) |
42(42%) |
> 0.05 |
| Night sweat |
23(65.7%) |
49(49%) |
> 0.05 |
| Weight loss |
13(37.1%) |
14(14%) |
0.003 |
| Anorexia |
17(48.6%) |
25(25%) |
> 0.05 |
| Headache |
8(22.9%) |
23(23%) |
> 0.05 |
| Arthralgia |
20(57.15) |
53(53%) |
> 0.05 |
| Myalgia |
16(45.7%) |
36(36%) |
> 0.05 |
| Vertebral tenderness |
35(100%) |
0 |
- |
Moreover, 54.28% of the patients with BS had erythrocyte sedimentation rate (ESR) ≥50 mm/h, but 18% of them without BS had ESR ≥ 50 mm/h. Therefore, there were statistically significant differences between the patients with and without BS concerning the mean ESR (mm/h) and C-reactive protein (CRP) (qualitative) (Table 3). The frequencies for spondylodiscitis in patients having weight loss, anorexia, and high CRP were significantly higher compared to the patients with absence of the given variables (Table 4). Linear-by-linear association chi square test showed that the increase in CRP was significantly associated with higher spondylodiscitis (54.2% for CRP =+++, 42.1% for CRP =++, 11.4% for CRP =+ and 5.3% for CRP = negative) (P for trend < 0.0001). In multiple logistic regression analysis, age (odds ratio [OR] = 1.032; P = 0.034) and CRP (OR = 8, P= 0.006) were discovered to be the significant predictors after adjustment for other variables.
Table 3.
Comparison of Laboratory Findings Between Brucellosis Patients With and Without Spondylodiscitis
|
Laboratory findings
|
Brucellosis patients
|
P-
value
|
With spondylitis
(n=35)
|
Without spondylitis
(n=100)
|
WBC(cells/µl)
Mean ±SD |
7754.28±2845.46 |
6304±1996.45 |
0.008 |
Hb (g/dl)
Mean ±SD |
12.64±1.79 |
12.69±1.63 |
0.860 |
ESR (mm/h)
Mean ±SD |
56.85±24.82 |
31.04±23.95 |
< 0.001 |
Platelet(cells/µl)
Mean ±SD |
194571±68919.51 |
219820±67531.41 |
0.06 |
AST(U/L)
Mean ±SD |
41.82±29.63 |
38.75±33.66 |
0.632 |
ALT(U/L)
Mean ±SD |
48.37±41.95 |
49.51±76.25 |
0.933 |
ALP(IU/L)
Mean ±SD |
219.03±127.5 |
249.03±169.35 |
0.341 |
CRP (Qualitative)
≤1+
≥ 2+ |
7(20%)
28(80%) |
68(68%)
32(32%) |
< 0.001 |
Table 4.
Factors associated significantly with spondylodiscitis in 135 patients with brucellosis
|
Predictors
|
Percentage of subjects (%)
|
Unadjusted OR
(95% CI)
|
P-
value
|
| Weight loss |
|
|
|
| Yes |
48.1 |
3.63(1.4-8.8) |
0.003 |
| No |
20.4 |
1 |
|
| CRP |
|
|
|
| Positive |
34 |
9.28(2.1-40.9) |
0.001 |
| Negative |
5.3 |
1 |
|
| Anorexia |
|
|
|
| Yes |
40.5 |
2.83(1.2-6.3) |
0.01 |
| No |
19.4 |
1 |
|
According to the spinal MRI reports, lumbar spines were affected most commonly (85.7%), followed by thoracic vertebrae (17.1%), sacral 5 (14.2%), and cervical zero. The most common vertebral involvement was L4-L5 (45.7%). Some of the patients with BS had more than one site of involvement in their spine.
The most common radiological findings in the spine MRI among the patients with spondylodiscitis were erosion at the anterosuperior portion of vertebral bodies 27 (77.1%), narrowing of the disc space between the two vertebrae 20 (57.1%), diskitis 10 (28.6%), vertebral body destruction 10 (28.6%), epiphysitis 5 (14.3%), paravertebral and epidural abscess 2 (5.7%), and involvement of more than two sites 7 (20%).
Figure 1 and 2 present the information about a 21-year-old woman with BS and paravertebral abscess as well as a 47-year-old man with spondylodiscitis and paravertebral abscess.
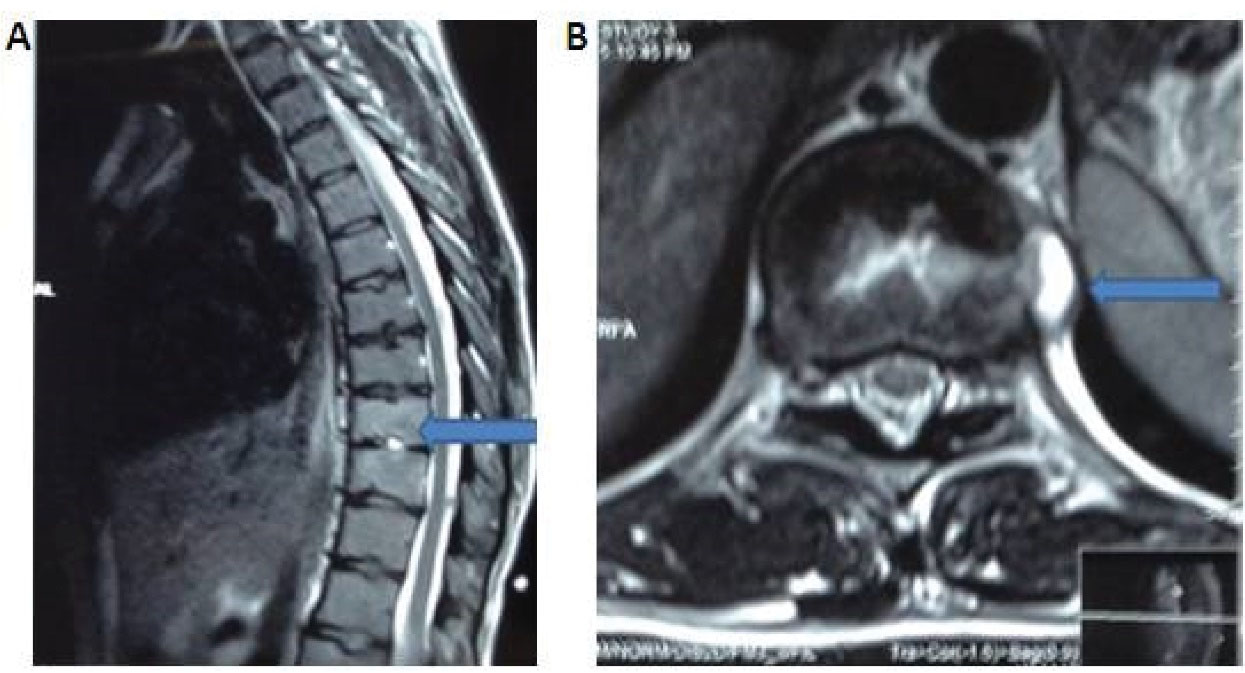
Figure 1.
Spinal MRI of a 21-year-old Woman With Back and Joints Pain From 2 Months Before Admission. A, The arrow indicates bone marrow edema in T9 and T10 Body With Central Necrosis in T9-T10 Disc Compatible With Spondylodiscitis. B, The Arrow Indicates Left Paravertebral Collection Compatible With Paravertebral Abscess
.
Spinal MRI of a 21-year-old Woman With Back and Joints Pain From 2 Months Before Admission. A, The arrow indicates bone marrow edema in T9 and T10 Body With Central Necrosis in T9-T10 Disc Compatible With Spondylodiscitis. B, The Arrow Indicates Left Paravertebral Collection Compatible With Paravertebral Abscess
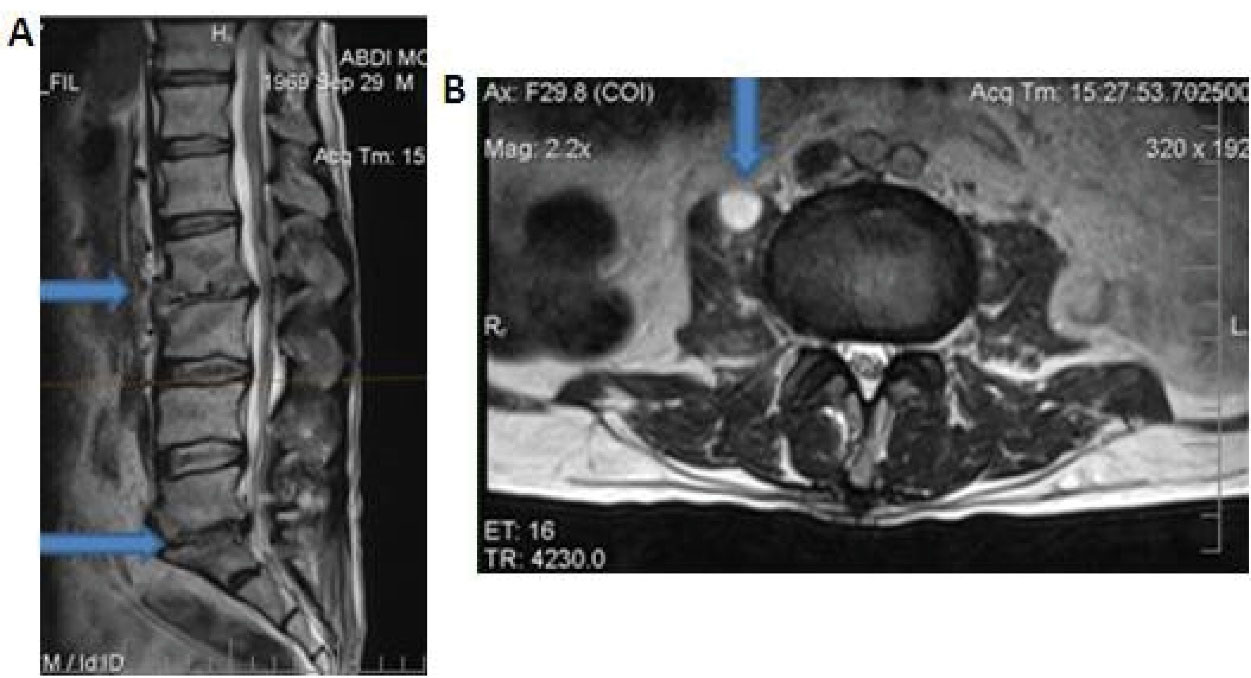
Figure 2.
Spinal MRI of a 47-year-old Man With Low Back Pain and Radiculopathy From 2 Months Before Admission. A, The Arrows Indicate Erosion at the Antrosuperior Portion of L2-L3 and L5-S1 Vertebral Bodies and Narrowing of the Disc Space Between Vertebrae. B, The Arrow Indicates a Paravertebral Abscess in L2 Spine
.
Spinal MRI of a 47-year-old Man With Low Back Pain and Radiculopathy From 2 Months Before Admission. A, The Arrows Indicate Erosion at the Antrosuperior Portion of L2-L3 and L5-S1 Vertebral Bodies and Narrowing of the Disc Space Between Vertebrae. B, The Arrow Indicates a Paravertebral Abscess in L2 Spine
Discussion
Brucellosis may affect various body organs, but spondylitis is the most common complication of brucellosis with the incidence rates ranging from 2 to 60% (1,12-14). BS is more common in older patients with brucellosis, and the lumbar vertebrae are commonly affected spinal sites in BS (1). In the present study, the patients with BS were older than those without it. Similar studies have reported spondylitis as the most common complication of brucellosis in the elderly (5,7-9,15-17).
A previous study carried out in Hamadan, Iran,showed that 28.6% of brucellosis patients had osteoarticular complications, and spondylitis was reported in 21.4% of them (5). In a study by Guler et al (8),however, 48.3% of the patients had osteoarticular complications and 88.26% of them had spondylitis; these percentages were higher than those found in our study. In our study, 70.37% of all patients were from rural areas and 38.5% of them had a positive family history; while in Guler et al study (8), only 50.4% of the patients were from rural areas and 22% of them had a positive family history. In the study by Smailnejad Gangi et al (9), on the other hand, 74% of the patients were from rural residents. The differences between our results and those from the given studies may have been attributed to the fact that more rural populations resided in Hamadan province. According to our study results, no significant differences were detected between patients with and without BS in terms of sex, neighborhood, occupation, history of contact with domestic animals, consumption of unpasteurized dairy products, previous brucellosis, and brucellosis in family members, which were consistent with findings from Koubaa et al study (7). In Smailnejad Gangi et al (9) study, the main risk factors for brucellosis were sheepherders and the consumption of unpasteurized dairy products; in our study, however, 100% of the patients with BS had consumed unpasteurized dairy products and 60% of them had contacts with domestic animals. In the study by Gokhale et al (10), the main risk factors were identified as being the consumption of unpasteurized dairy products and, similar to our study, the contacts with infected animals which had afflicted 60% of the patients. In another study by Gokhale et al (10), all patients had the history of contacting with infected animals and consuming unpasteurized dairy products.
In our study, the most common clinical manifestations in the patients with BS were back pain, vertebral tenderness, and fever, respectively, which were similar to the manifestations reported by Koubaa et al (7), Gokhale et al (18), and Bodur et al (17). In addition, vertebral tenderness were observed in all patients with BS in the studies by Ariza et al (19) and Namiduru et al (15), which were the same manifestations found in our study.
In contrast, Smailnejad Gangi et al (9) reportedsweating, fever, and arthralgia as the most common symptoms in the patients. In the studies by Koubaa et al (7) and Smailnejad Gangi et al (9), the duration of symptoms before diagnosis in patients with BS were 72 and 67 days, respectively, which was consistent with the duration found in our study. The main problem to early diagnosis of BS was the nonspecific and subtle manifestations of symptoms and signs, especially those manifested in older patients suffering from degenerative joint disorders.
In our study, the most common sites of spine involvements in the patients with BS were lumbar 30(85.7%) and thoracic (17.1%). As for other studies, the most common site of spine involvement in the patients with BS was lumbar (7,9,10,15,17,20,21).
In the present study, ESR in the patients with BS was significantly higher than that in the patients without BS, which was similar to that found in the studies by Koubaa et al (7), Smailnejad Gangi et al (9), Gokhale et al (10), Namiduru et al (15), Aktug-Demir et al (16), and Bodur et al (17).
In addition, CRP as a biomarker of inflammation, which is commonly positive in brucellosis, was higher in the patients with BS than that observed in those without BS. No data for CRP on the patients with BS were reported by other studies compare to ours.
Paravertebral or epidural masses were detected in 5.7% of the patients with BS, which was in line with results from some other studies in this regard (9,10,17,20,21). According to the results from Ariza et al (19) study, whole body bone scan with TC99 was positive in all patients, which was consistent with our study findings. In the present study, no significant difference was observed between the patients with and without BS regarding the mean of hemoglobin, platelet, WBC count, and liver function tests, which was in agreement with the finding from Namiduru et al (15) study. In Turgut et al (21) study, the most common radiological findings were the narrowing of the disc space between the two vertebrae and vertebral body destruction. In our study, on the other hand, erosion at the anterosuperior portion of vertebral bodies (77.1%), narrowing of the disc space between the two vertebrae (57.1%), diskitis (28.6%), and vertebral body destruction (28.6%) were seen on spinal MRI of the patients with BS.
The present study had some limitations. First, hospital-based and ambulatory patients were not included in this study; therefore, some patients with BS might have been missed. Second, the results of the treatment and follow-up of the patients had not been recorded in their medical records and, therefore, we were not able to obtain the data on later development in patients’ conditions.
Conclusions
According to our study results, spondylodiscitis was found to be a serious complication of brucellosis and more common in older patients. The most common site of vertebral involvement was lumbar vertebrae. Therefore, it is recommended that BS be considered in the differential diagnosis of the patients with prolonged fever, low back pain, and lumbosacral vertebrae tenderness in the endemic areas.
Authors’ Contribution
We confirm that the manuscript as well as the order of authors listed in the manuscript were contributed, reviewed, and approved by all named authors.
Ethical Approval
This study was approved by the ethical committee of Hamadan University of Medical Sciences (IR.SBMU. RETECH. REC.1397.246), and all participants were asked to sign an informed consent prior to enter the study.
Conflict of Interests
The authors declare no conflict of interests.
Funding/Support
This study received no financial support.
Acknowledgement
The authors would like to thank all medical staff of Infectious Diseases Ward for helping us the collect the data. This study was derived from an MD thesis at Hamadan University of Medical Sciences.
References
- Gul HC, Erdem H. Brucella species. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 8th ed. Philadelphia: Churchill Livingstone; 2015. p. 2584-9.
- Zeinali M, Nabavi M, Shirzadi MR, Hajrasoliha H. Epidemiological situation of brucellosis in the past three decades in Iran. Iranian J Public Health 2014; 43(2):24. [ Google Scholar]
- Afsharpaiman S, Mamishi S. Brucellosis: review of clinical and laboratory features and therapeutic regimens in 44 children. Acta Med Iran 2008; 46(6):489-94. [ Google Scholar]
- Salari MH, Khalili MB, Hassanpour GR. Selected epidemiological features of human brucellosis in Yazd, Islamic Republic of Iran: 1993-1998. East Mediterr Health J 2003; 9(5-6):1054-60. [ Google Scholar]
- Hashemi SH, Keramat F, Ranjbar M, Mamani M, Farzam A, Jamal-Omidi S. Osteoarticular complications of brucellosis in Hamedan, an endemic area in the west of Iran. Int J Infect Dis 2007; 11(6):496-500. doi: 10.1016/j.ijid.2007.01.008 [Crossref] [ Google Scholar]
- Hajia M, Rahbar M, Keramat F. Epidemiological, clinical, diagnostic and treatment aspects of hospitalized brucellosis patients in Hamadan. Ann Trop Med Public Health 2009; 2(2):42-5. [ Google Scholar]
- Koubaa M, Maaloul I, Marrakchi C, Lahiani D, Hammami B, Mnif Z. Spinal brucellosis in South of Tunisia: review of 32 cases. Spine J 2014; 14(8):1538-44. doi: 10.1016/j.spinee.2013.09.027 [Crossref] [ Google Scholar]
- Guler S, Kokoglu OF, Ucmak H, Gul M, Ozden S, Ozkan F. Human brucellosis in Turkey: different clinical presentations. J Infect Dev Ctries 2014; 8(5):581-8. doi: 10.3855/jidc.3510 [Crossref] [ Google Scholar]
- Smailnejad Gangi SM, Hasanjani Roushan MR, Janmohammadi N, Mehraeen R, Soleimani Amiri MJ, Khalilian E. Outcomes of treatment in 50 cases with spinal brucellosis in Babol, Northern Iran. J Infect Dev Ctries 2012; 6(9):654-9. doi: 10.3855/jidc.2175 [Crossref] [ Google Scholar]
- Gokhale YA, Ambardekar AG, Bhasin A, Patil M, Tillu A, Kamath J. Brucella spondylitis and sacroiliitis in the general population in Mumbai. J Assoc Physicians India 2003; 51:659-66. [ Google Scholar]
- Beeching NJ, Corbel MJ. Brucellosis. In: Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 19th ed. New York: McGraw Hill; 2015. p. 1-5.
- Aydin G, Tosun A, Keles I, Ayaşlioglu E, Tosun O, Orkun S. Brucellar spondylodiscitis: a case report. Int J Clin Pract 2006; 60(11):1502-5. doi: 10.1111/j.1742-1241.2005.00656.x [Crossref] [ Google Scholar]
- Ugarriza LF, Porras LF, Lorenzana LM, Rodríguez-Sánchez JA, García-Yagüe LM, Cabezudo JM. Brucellar spinal epidural abscesses Analysis of eleven cases. Br J Neurosurg 2005; 19(3):235-40. doi: 10.1080/02688690500204949 [Crossref] [ Google Scholar]
- Lim HS, Song YG, Yoo HS, Park MY, Kim JW. Brucellosis: an overview. Korean J Epidemiol 2005; 27(1):26-36. [ Google Scholar]
- Namiduru M, Karaoglan I, Gursoy S, Bayazit N, Sirikci A. Brucellosis of the spine: evaluation of the clinical, laboratory, and radiological findings of 14 patients. Rheumatol Int 2004; 24(3):125-9. doi: 10.1007/s00296-003-0339-7 [Crossref] [ Google Scholar]
- Aktug-Demir N, Kolgelier S, Ozcimen S, Sumer S, Demir LS, Inkaya AC. Diagnostic clues for spondylitis in acute brucellosis. Saudi Med J 2014; 35(8):816-20. [ Google Scholar]
- Bodur H, Erbay A, Colpan A, Akinci E. Brucellar spondylitis. Rheumatol Int 2004; 24(4):221-6. doi: 10.1007/s00296-003-0350-z [Crossref] [ Google Scholar]
- Santiago T, Rovisco J, Silva J, Pereira da Silva JA. [Osteoarticular brucellosis: an analysis of the past decade]. Acta Reumatol Port 2011; 36(2):120-5. [ Google Scholar]
- Ariza J, Gudiol F, Valverde J, Pallarés R, Fernández-Viladrich P, Rufí G. Brucellar spondylitis: a detailed analysis based on current findings. Rev Infect Dis 1985; 7(5):656-64. doi: 10.1093/clinids/7.5.656 [Crossref] [ Google Scholar]
- Gu L, Yu QT, Zang WY, Xu DH. [Value of magnetic resonance imaging in diagnosis of brucellar spondylitis]. Zhongguo Gu Shang 2012; 25(5):433-5. [ Google Scholar]
- Turgut M, Turgut AT, Koşar U. Spinal brucellosis: Turkish experience based on 452 cases published during the last century. Acta Neurochir (Wien) 2006; 148(10):1033-44. doi: 10.1007/s00701-006-0877-3 [Crossref] [ Google Scholar]