Avicenna Journal of Clinical Microbiology and Infection. 7(2):56-59.
doi: 10.34172/ajcmi.2020.12
Original Article
The Considerable Cases of Imported Malaria in Larestan in the South of Iran During 2008-2018
Forogh Ebrahimizadeh 1  , Gholamreza Shokoohi 1, Fatemeh Sahranavard 1, Ahmad Abolghazi 1, 2, *
, Gholamreza Shokoohi 1, Fatemeh Sahranavard 1, Ahmad Abolghazi 1, 2, * 
Author information:
1Department of Medical Parasitology, Jahrom University of Medical Sciences, Jahrom, Fars, Iran.
2Zoonoses Research Center, Jahrom University of Medical Sciences, Jahrom, Iran.
Abstract
Background: Malaria is one of the fatal parasitic diseases caused by a species of Plasmodium parasite. The disease is found worldwide, and Plasmodium vivax, P. falciparum, P. ovale, P. malariae, and P. knowlesi are the common causes among which P. vivax and P. falciparum are numerous general malaria-causing species in the world. Therefore, the present research aimed at determining the extent of these cases over the past few years in one of the southern regions of Larestan, located in Fars province, Iran.
Methods: The population of the study included people referring to health centers between 2008 and 2018 whose data were recorded in the health centers of Larestan county. Data collection and evaluation were performed through patient files and recorded information.
Results: The entire number of recorded malaria cases from 2008 to 2018 was 156, from which 140 (89.8%) and five (2.3%) cases were related to P. vivax and P. falciparum, and 11 mixed cases (7%) were reported as well.
Conclusions: Over the years, malaria eradication has been a significant problem for countries. Therefore, it is important to find out the intervening factors such as relapse and imported malaria. Hence, considering the reduced imported malaria is required for eradicating this disease.
Keywords: Imported, Malaria, Larestan, Iran
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Background
Malaria is considered as one of the most significant health difficulties in the world, notably in developing countries and tropical areas, which is caused by a blood-borne parasite called Plasmodium and is often transmitted through the bites of Anopheles mosquitos (1). The disease is also transmitted through blood transfusion using a common syringe, organ transplantation, and from the mother to the fetus through the placenta (1,2). In addition, P. vivax, P. falciparum, P. ovale, P. malariae, and P. knowlesi are the species of Plasmodium that lead to malaria in people. Among these species, P. vivax is the most common type and P. falciparum is the most severe and most dangerous one (3,4). The three species of P. vivax, P. falciparum, and P. malariae exist in Iran (4). Approximately half of the world community lived at the risk of malaria in 2017. More precisely, there were 219 million malaria cases and malaria deaths have been 435,000 in this year (5). Some population groups such as children under the age of five, pregnant women, infants, HIV/AIDS patients, non-immune immigrants, and travelers are at the higher risk and develop the disease more severely compared to other people (6). The complications of this disease include affecting cerebral malaria, respiratory and renal systems or hemorrhage, metabolic acidosis, and hypoglycemia (7-9). One of the dominant problems in fighting malaria in Iran has been illegal immigration from neighboring countries such as Afghanistan and Pakistan to Iran while malaria was native in these countries and entered the southern areas of the country by these immigrants (10). Malaria has a declining trend in Iran and is mostly reported in the southern regions of Iran, especially in Sistan and Baluchestan, Kerman, and Bushehr provinces. Larestan is also located in the south of Iran near Bushehr and Jahrom, and the trend of this disease is decreasing in these cities (5). It should be noted that malaria is endemic in Iran, especially in the southern regions of the country. Considering the favorable weather conditions of this region for the survival of the life cycle of malaria and the entrance of illegal immigrants from neighboring countries, studying the prevalence and epidemiology of this disease in malaria-endemic regions of Iran has always been of importance. Accordingly, the current study focused on identifying the extent of these cases over the past few years in one of the southern regions of Larestan, located in Fars Province, Iran.
Methods
The present cross-sectional study was conducted in Larestan county. It is placed in the south of Fars province in 915 m over the sea level with an area of 30 960 km2. According to the most recent census data of the country (2016), this county has a population of about 226 879 people and consists of nine cities of Lar, Banaruiyeh, Evaz, Beyram, Fishvar, Juyom, Khur, Latifi, and Emad Deh (11). The study population included all malaria suspected cases who referred to health centers during 2008-2018 and had recorded data in the health centers of Larestan county. All samples were identified by blood smears and Giemsa staining and then diagnosed by a malaria expert using an optical microscope. In addition, data analysis and collection were conducted through patient files and recorded information. In this research, parameters such as the patient’s gender, age, symptoms, and place of residence were used, and finally, the data were analyzed using SPSS software.
Results
The total number of reported cases of malaria was 156 (2008-2018), of which 140 cases (89.8%) were related to P. vivax, 5 cases (3.2%) belonged to P. falciparum, and 11 cases (7%) were of mixed type. Further, 101 cases (64.75%) and 55 (35.25%) cases were males and females, respectively. Furthermore, 130 (83.33%) out of s total of 156 patients reported that cases were imported and 26 cases (16.66%) were relapsed. Moreover, the highest numbers of cases (32.7%) were in the range of 31-40 years old (Table 1). Finally, fever was the most common clinical symptom in patients. Other clinical signs are listed in Table 2.
Table 1.
The Age Group of Patients With Malaria in Larestan in the South of Iran From 2008 to 2018
|
Age
|
Number
|
Percent
|
| 0-10 |
11 |
7 |
| 11-20 |
17 |
10.9 |
| 21-30 |
46 |
29.5 |
| 31-40 |
51 |
32.7 |
| >40 |
31 |
19.9 |
Table 2.
The Most Common Clinical Symptom of Patients With Malaria in Larestan in the South of Iran From 2008 to 2018
|
Signs of Malaria
|
Number
|
Percent
|
| Chills |
29 |
18.6 |
| Fever |
112 |
71.8 |
| Sweating |
32 |
20.5 |
| Anemia |
33 |
21.1 |
| Hypoglycemia |
28 |
18 |
| Hypotension |
81 |
52 |
| Jaundice |
12 |
7.7 |
| Dark urine |
7 |
4.5 |
Among these 156 cases, 1 (0.6%) case had Iranian nationality, 5 cases (3.2%) were Pakistani immigrants, and the remaining 150 cases (96.2%) were Afghan immigrants (Figures 1 and 2).
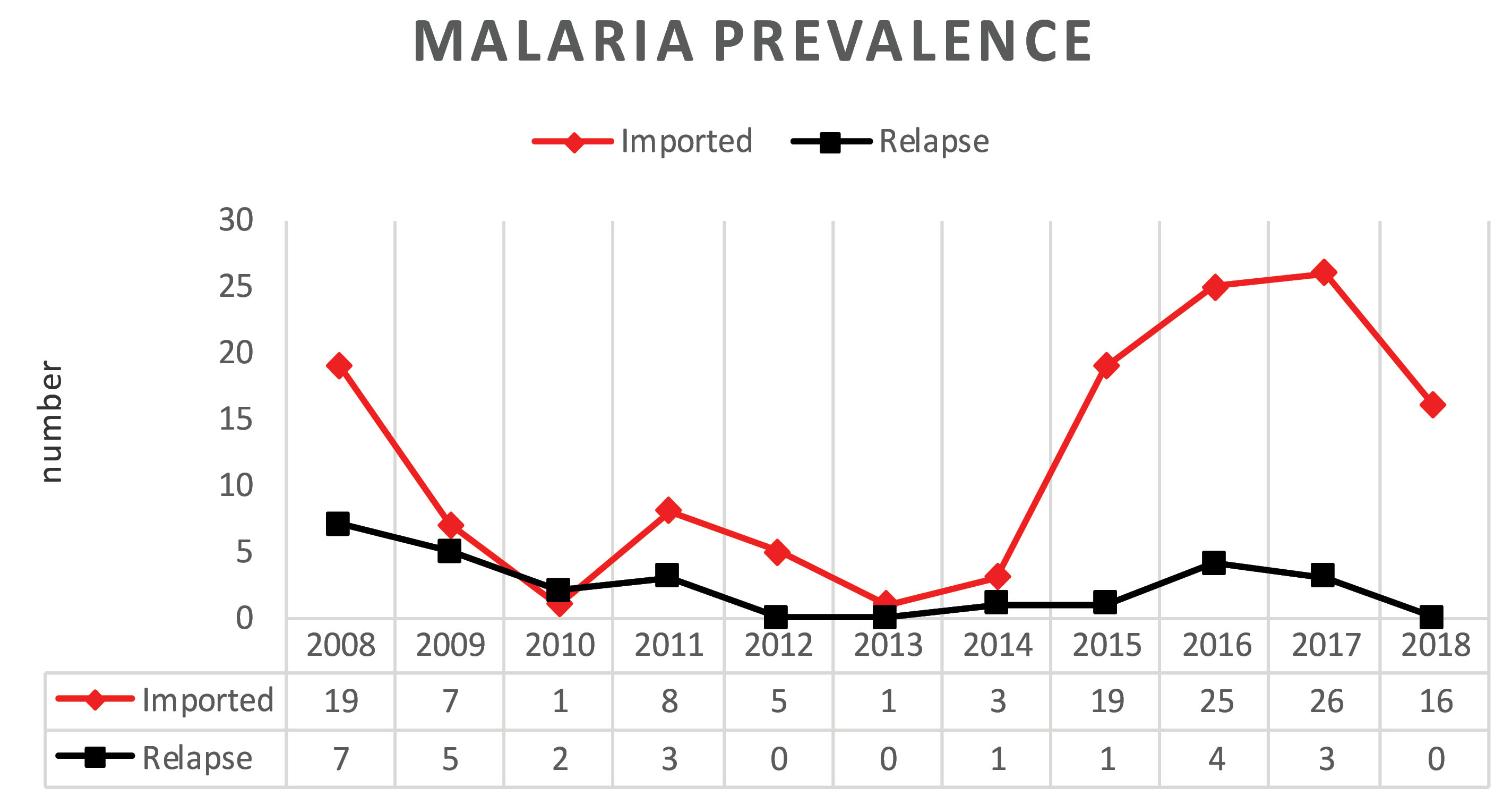
Figure 1.
The Frequency of the Relapsed and Imported Cases of Malaria in Larestan in the South of Iran From 2008 to 2018.
.
The Frequency of the Relapsed and Imported Cases of Malaria in Larestan in the South of Iran From 2008 to 2018.
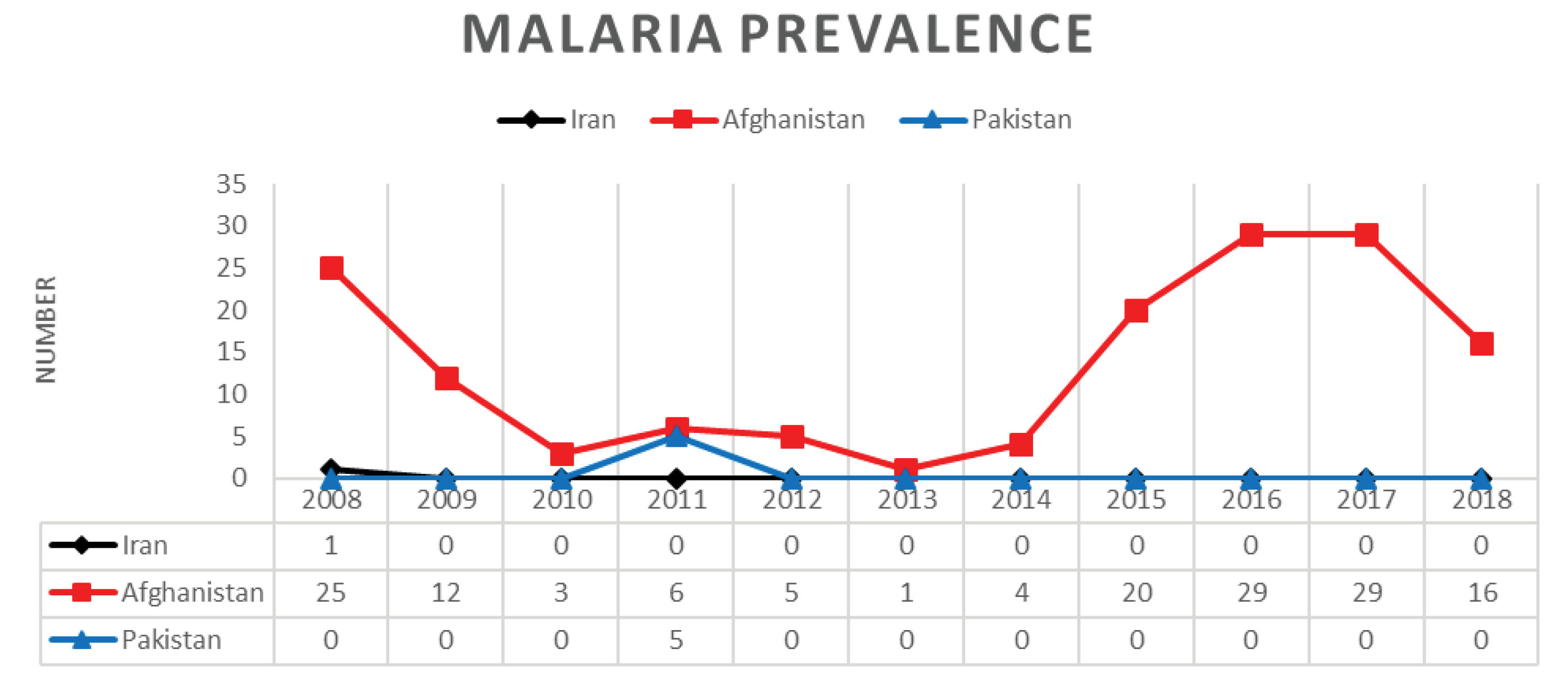
Figure 2.
The Frequency of Malaria Based on Nationality in Larestan in the South of Iran From 2008 to 2018.
.
The Frequency of Malaria Based on Nationality in Larestan in the South of Iran From 2008 to 2018.
Discussion
Due to high mortality and the complications of malaria as one of the dangerous parasitic diseases worldwide, especially in susceptible countries, finding an appropriate method to control and prevent the disease has permanently been important (12,13). Regions struggling for intercepting and eliminating malaria have continuously attempted to fight the causes of malaria increase and recurrence in the region. Several factors increase or decrease the incidence of infectious diseases such as leishmaniasis and malaria in a region (14). In addition, relapse and imported malaria are the factors that change the trend of malaria prevalence in a region (15-17). Iran is not an exception in this regard and the fact that it is currently in the process of eliminating malaria and implementing the eradication plan by 2020 further highlights the importance of this issue. Therefore, finding the cases of relapse, especially imported malaria, can accommodate this program greatly. Thus, if the two factors are not taken into account, the eradication project in a region will be defeated and it may also be impossible (18,19). Hence, the accurate understanding of the number of cases and imported malaria in addition to reflecting the health status of malaria reflects our success in achieving the main goal of disease eradication in 2020. The present research aimed to identify the extent of these cases over the past few years in one of the southern regions of Larestan, Fars, Iran. As regards gender, the number of reported cases was higher in men compared to women, which is consistent with the results of Piroozi et al (20). Accordingly, higher male suffering compared to women was justified by 155 cases (approximately 94.4% of malaria cases) who were illegal immigrants from Afghanistan and Pakistan, and in most cases, were men who immigrated to Iran for work. The majority of these immigrants moved to Iran due to bad economic conditions in their country in order to find a suitable job. Among 156 reported cases, 140 (89.8%) and 5 (3. 2%) cases were related to P. vivax and P. falciparum, respectively, indicating that P. vivax is predominant in Iran. This is in line with the findings of previous studies by Edrissian et al, Kazemi et al, and Khalili et al (21-23). Of the total reported cases, 130 cases (83.33%) were those from imported malaria, and the remaining cases were reported as relapses, representing the high rate of imported malaria, which corroborates with the results of some studies conducted in different parts of the country in recent years (21,24). In the last ten years, only one case (0.6%) was reported by the residents of the region in 2008 and 155 cases representing more than 94.4% of the total cases included Afghani and Pakistani immigrants among which, the number of Afghans was higher, which matches the findings of several studies performed in different parts of the country in recent years (16,21,25,26). The higher rate of imported malaria indicated high risk in the southern areas of the country. Moreover, the evasion of law by immigrants, especially Afghans, led to the transmission of the disease through importation and threatening the country as a potential source of risk in terms of malaria. Therefore, it is highly necessary to take specific measures to eliminate or reduce this risk. Furthermore, by interrupting the internal cycle in areas with all proper climate and geographic conditions, the presence of numerous carriers in these areas and the interruption of the life cycle of the parasite have gradually reduced the relative safety of the inhabitants of the area toward the disease (26,27). All these factors make the inhabitants of these areas at a higher risk of the prevalence of malaria and jeopardize their health. On the other hand, an increase in reports on the resistance of the Plasmodium parasite and the malaria carrier to the poisons and existing drugs is a warning to the health against malaria in areas that have eradicated malaria and malaria-free areas (25-28).
Conclusions
After eliminating and eradicating malaria, the mission of maintaining this eradication is even more significant throughout the world, which alarms global health officials to adopt an appropriate strategy for maintaining malaria eradication.
Conflict of Interests
All authors have no conflict of interests to declare.
References
- Kitchen AD, Chiodini PL. Malaria and blood transfusion. Vox Sang 2006; 90(2):77-84. doi: 10.1111/j.1423-0410.2006.00733.x [Crossref] [ Google Scholar]
- Slinger R, Giulivi A, Bodie-Collins M, Hindieh F, John RS, Sher G. Transfusion-transmitted malaria in Canada. CMAJ 2001; 164(3):377-9. [ Google Scholar]
- Triglia T, Healer J, Caruana SR, Hodder AN, Anders RF, Crabb BS. Apical membrane antigen 1 plays a central role in erythrocyte invasion by Plasmodium species. Mol Microbiol 2000; 38(4):706-18. doi: 10.1046/j.1365-2958.2000.02175.x [Crossref] [ Google Scholar]
- Ebrahimzadeh A, Fouladi B, Fazaeli A. High rate of detection of mixed infections of Plasmodium vivax and Plasmodium falciparum in South-East of Iran, using nested PCR. Parasitol Int 2007; 56(1):61-4. doi: 10.1016/j.parint.2006.12.001 [Crossref] [ Google Scholar]
- World Health Organization (WHO). World Malaria Report 2018. WHO; 2018. https://www.who.int/malaria/publications/world-malaria-report-2018/en/.
- Hay SI, Guerra CA, Tatem AJ, Noor AM, Snow RW. The global distribution and population at risk of malaria: past, present, and future. Lancet Infect Dis 2004; 4(6):327-36. doi: 10.1016/s1473-3099(04)01043-6 [Crossref] [ Google Scholar]
- Zingman BS, Viner BL. Splenic complications in malaria: case report and review. Clin Infect Dis 1993; 16(2):223-32. doi: 10.1093/clind/16.2.223 [Crossref] [ Google Scholar]
- Millan JM, San Millan JM, Muñoz M, Navas E, Lopez-Velez R. CNS complications in acute malaria: MR findings. AJNR Am J Neuroradiol 1993; 14(2):493-4. [ Google Scholar]
- Murphy SC, Breman JG. Gaps in the childhood malaria burden in Africa: cerebral malaria, neurological sequelae, anemia, respiratory distress, hypoglycemia, and complications of pregnancy. Am J Trop Med Hyg 2001; 64(1-2 Suppl):57-67. doi: 10.4269/ajtmh.2001.64.57 [Crossref] [ Google Scholar]
- Zakeri S, Najafabadi ST, Zare A, Djadid ND. Detection of malaria parasites by nested PCR in south-eastern, Iran: evidence of highly mixed infections in Chahbahar district. Malar J 2002; 1:2. doi: 10.1186/1475-2875-1-2 [Crossref] [ Google Scholar]
- Larestan County. Wikipedia site. Available from: https://en.wikipedia.org/wiki/Larestan_County.
- Greenwood BM. The microepidemiology of malaria and its importance to malaria control. Trans R Soc Trop Med Hyg 1989; 83 Suppl:25-9. doi: 10.1016/0035-9203(89)90599-3 [Crossref] [ Google Scholar]
- Thomasin C, Corradin G, Men Y, Merkle HP, Gander B. Tetanus toxoid and synthetic malaria antigen containing poly(lactide)/poly(lactide-co-glycolide) microspheres: importance of polymer degradation and antigen release for immune response. J Control Release 1996; 41(1-2):131-45. doi: 10.1016/0168-3659(96)01363-6 [Crossref] [ Google Scholar]
- Macdonald G. The Epidemiology and Control of Malaria. London: Oxford University Press; 1957.
- Raghavendra K, Barik TK, Reddy BP, Sharma P, Dash AP. Malaria vector control: from past to future. Parasitol Res 2011; 108(4):757-79. doi: 10.1007/s00436-010-2232-0 [Crossref] [ Google Scholar]
- Abolghazi A, Ebrahimizadeh F, Sharafi F, Hatami N, Vafai Z. A declining trend of leishmaniasis based on previous data in Larstan, South of Iran 2007-2017. Ann Glob Health 2019; 85(1). doi: 10.5334/aogh.1539 [Crossref]
- Takken W, Knols BG. Malaria vector control: current and future strategies. Trends Parasitol 2009; 25(3):101-4. doi: 10.1016/j.pt.2008.12.002 [Crossref] [ Google Scholar]
- World Health Organization (WHO). Update on the E-2020 Initiative of 21 Malaria-Eliminating Countries. WHO; 2018.
- Soofi K, Khanjani N, Kamiabi F. The Challenges of the malaria elimination program in the south east of Iran: a qualitative study. J Arthropod Borne Dis 2019; 13(1):94-103. [ Google Scholar]
- Piroozi B, Moradi G, Safari H, Faraji L, Sadi S, Alinia C, Raeisi A. Incidence, mortality, and burden of malaria and its geography-ical distribution in Iran during 2002-2015. Iran J Public Health 2019; 48(Suppl 1):53-61. [ Google Scholar]
- Edrissian G. Malaria in Iran: past and present situation. Iran J Parasitol 2006; 1(1):1-14. [ Google Scholar]
- Kazemi F, Fallahizadeh S, Allasvand R, Arjmand R. Epidemiology of malaria in Ramhormoz county, Southwest of Iran, during 2001-2016. Int J Biomed Public Health 2018; 1(2):67-70. doi: 10.22631/ijbmph.2018.61058 [Crossref] [ Google Scholar]
- Khalili MB, Anvari Tafti MH, Sadeh M. Epidemiological pattern of malarial disease in the province of Yazd, Iran (since 1986-2006). World J Med Sci 2009; 4(1):41-45. [ Google Scholar]
- Norouzinejad F, Ghaffari F, Raeisi A, Norouzinejad A. Epidemiological status of malaria in Iran, 2011-2014. Asian Pac J Trop Med 2016; 9(11):1055-61. doi: 10.1016/j.apjtm.2016.09.007 [Crossref] [ Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Oshaghi MA, Haghdoost AA, Shahi M, Sedaghat MM. Entomological and epidemiological attributes for malaria transmission and implementation of vector control in southern Iran. Acta Trop 2012; 121(2):85-92. doi: 10.1016/j.actatropica.2011.04.017 [Crossref] [ Google Scholar]
- Abolghazi A, Heidari A, Moin-Vaziri V, Haghighi A, Seyyed Tabaei SJ, Keshavarz H. Genetic diversity in C-terminal of SERA5 gene in the blood stage of human isolates of Plasmodium vivax in Sistan and Baluchistan, Iran. Iran J Parasitol 2018; 13(3):440-7. [ Google Scholar]
- Smith T, Felger I, Tanner M, Beck HP. Premunition in Plasmodium falciparum infection: insights from the epidemiology of multiple infections. Trans R Soc Trop Med Hyg 1999; 93 Suppl 1:59-64. doi: 10.1016/s0035-9203(99)90329-2 [Crossref] [ Google Scholar]
- Obi RK, Okangba CC, Nwanebu FC, Ndubuisi UU, Orji NM. Premunition in Plasmodium falciparum malaria. Afr J Biotechnol 2010; 9(10):1397-401. doi: 10.5897/AJBx09.034 [Crossref] [ Google Scholar]