Avicenna Journal of Clinical Microbiology and Infection. 10(4):137-144.
doi: 10.34172/ajcmi.3497
Original Article
Following WHO Guidelines to Respond to a Water Contamination Outbreak in the Edge of Hamadan, West of Iran
Fateme Torkaman Asadi 1  , Lida Rafati 2, Fahime Moeini 3, Salman Khazaei 4
, Lida Rafati 2, Fahime Moeini 3, Salman Khazaei 4  , Taghi Taghi Hajilouei 3, Mahdi Khodabakhshi 3, Masoumeh Javaheri 3, *
, Taghi Taghi Hajilouei 3, Mahdi Khodabakhshi 3, Masoumeh Javaheri 3, * 
Author information:
1Infectious Diseases Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
2Environment and Work Health Management, Vice-Chancellor for Health, Hamadan University of Medical Sciences, Hamadan, Iran
3Deputy of Health, Hamadan University of Medical Sciences, Hamadan, Iran
4Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: Water and foodborne disease outbreaks continually present formidable challenges to healthcare systems, leading to morbidity, mortality, and substantial economic losses. Investigating and reporting these outbreaks play a pivotal role in effectively controlling and mitigating future occurrences. This study endeavors to scrutinize an outbreak of water contamination in Mariyanaj, Hamadan, Iran, employing the World Health Organization’s (WHO’s) comprehensive 10-step framework.
Methods: In this descriptive study, we meticulously adhered to the WHO outbreak investigation and reporting guidelines, systematically progressing through each step to investigate and report the outbreak. Symptom/exposure samples, involving two samples per symptomatic individual, were collected and sent to the Center for Disease Control’s laboratory for examination. Additionally, we executed a case-control study (Step 7) to discern the root cause of the outbreak.
Results: The outbreak affected 919 individuals among 12115 residents of Mariyanaj city, with a male prevalence of 57.7%. The most impacted age group was 10-14 years. Predominant symptoms included abdominal pain, nausea, and vomiting. Through meticulous field investigations and the case-control study, the contaminated water source was identified. Human samples exhibited Escherichia coli and norovirus as the most prevalent pathogens, with E. coli also detected in water samples.
Conclusion: Despite advancements in outbreak investigation and reporting systems, the utilization of a standardized step-by-step approach proves more effective in identifying and managing outbreaks. The consistent monitoring of drinking water quality, particularly in times of water crises, emerges as a crucial factor in significantly preventing waterborne diseases.
Keywords: Waterborne disease outbreak, World Health Organization framework, Escherichia coli, Norovirus pathogens, Mariyanaj, Hamadan, Iran
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Please cite this article as follows: Torkaman Asadi F, Rafati L, Moeini F, khazaei S, Hajilouei T, Khodabakhshi M, et al. Following WHO guidelines to respond to a water contamination outbreak in the edge of Hamadan, west of Iran. Avicenna J Clin Microbiol Infect. 2023; 10(4):137-144. doi:10.34172/ajcmi.3497
Introduction
In developed nations, over 10% of the population experiences water and foodborne zoonotic diseases annually (1). Understanding the quality and quantity of water and its procurement is pivotal for optimizing consumption. Ideally, drinking water should be free from disease-causing microorganisms. To prevent disease transmission, it is customary to monitor water health and quality at every stage, from production to consumption. Consequently, a comprehensive assessment of water’s microbiological quality necessitates the examination of all potential pathogens causing human infections. Notably, the majority of environmentally transmitted diseases are linked to contaminated water and food, affecting an estimated 1.1 billion people globally. Eighty-eight percent of diarrheal diseases and 1.7 million annual deaths are attributed to the consumption of unsafe water and poor sanitation (2).
In developed countries, 30% of the population suffers from water and foodborne illnesses, while in developing nations, about 80% of all diseases and 33% of deaths stem from consuming contaminated water and food (3). This is primarily due to factors such as inadequate access to safe drinking water, diminishing groundwater levels, insufficient access to ample drinking water, declining annual rainfall, inadequate seasonal rainfall, and diminishing surface water levels, among others. According to the Centers for Disease Control and Prevention (CDC), a water and foodborne disease outbreak occurs when a group of people collectively consumes contaminated food, resulting in at least two or more individuals falling ill (4). Bacteria, parasites, viruses, and prions are the causative agents of these diseases (5).
Acute gastroenteritis, characterized by the sudden onset of diarrhea with or without vomiting, nausea, fever, or abdominal pain, is primarily caused by viruses (6). As mentioned earlier, contaminated water and food, often due to microorganisms such as parasites, viruses, and other pathogens are the primary cause of these outbreaks (7). In recent years, noroviruses have emerged as one of the most common pathogens leading to an increase in diarrhea when transmitted through drinking water (8). These disease outbreaks are a global challenge.
A five-year study on foodborne outbreaks in Iran from 2006 to 2011 revealed 2,250 foodborne outbreak reports, increasing from 0.07 per 100 000 people in 2006 to 1.38 per 100 000 people in 2011 (9). The pollution of water sources likely results from the lack of protection of water resources and the water supply system, as well as the direct release of pollution into the water sources of the area’s residents (9). Although there are no universal rules for determining the time when an outbreak occurs, three crucial factors in analyzing a disease outbreak are time, location, and affected individuals (6). Moreover, epidemiological studies play a significant role in identifying factors contributing to these outbreaks and planning for future prevention (10).
During a disease outbreak, key questions that need swift answers include: (a) What is the causative agent of the disease? (b) Where is the source or origin of the disease? (c) What has been the course of the disease outbreak over time? (11). Outbreaks of these diseases are pressing concerns for public health. The proper management of drinking water can prevent many diarrheal diseases in developing countries (12). A more detailed study based on the ten-step World Health Organization (WHO) outbreak investigation process includes confirming the occurrence of an outbreak, timely reporting and coordination with officials, collecting human and food samples for laboratory diagnosis, implementing control and prevention measures, organizing outbreak-related information, developing a hypothesis, designing and conducting an epidemiological study to test the hypothesis, analyzing collected data, interpreting findings, drawing conclusions, and presenting the findings of the outbreak investigation (13).
In September 2022, in the city of Mariyanaj with a population of approximately 12 115, several individuals presented symptoms such as abdominal pain, nausea, vomiting, fever, and occasional diarrhea. They sought medical attention at the Comprehensive Health Service Center of Mariyanaj. The rapid surge in the number of patients within a few hours created an emergency within the city’s healthcare system. In response, this study was conducted to identify and study the factors contributing to the outbreak in Mariyanaj and describe the affected individuals during September 2022, utilizing the ten-step process of outbreak investigation.
Materials and Methods
In September 2022, residents of Mariyanaj attended Ayatollah Bahari Hospital and local health centers with symptoms indicative of diarrhea and gastroenteritis. The number of affected individuals escalated over several days, raising concerns of an epidemic. Mariyanaj is situated in Hamadan County, with an urban population of 12 115 and a rural population covered by its health center totaling 9,464. Accordingly, this study aimed to investigate the outbreak’s epidemiology following the WHO’s ten-step outbreak investigation process.
Confirmation of an Outbreak
On Friday, September 4, 2022, at 14:40, a report from the Mariyanaj Comprehensive Health Services Center confirmed a surge in citizens with symptoms such as abdominal pain, non-bloody diarrhea, nausea, vomiting, stomach cramps, and low-grade fever (Figure 1). A rapid response team, including county health officials, university health deputies, and technical experts, gathered at Mariyanaj Comprehensive Health Center. The analysis of outbreak statistics substantiated its occurrence.
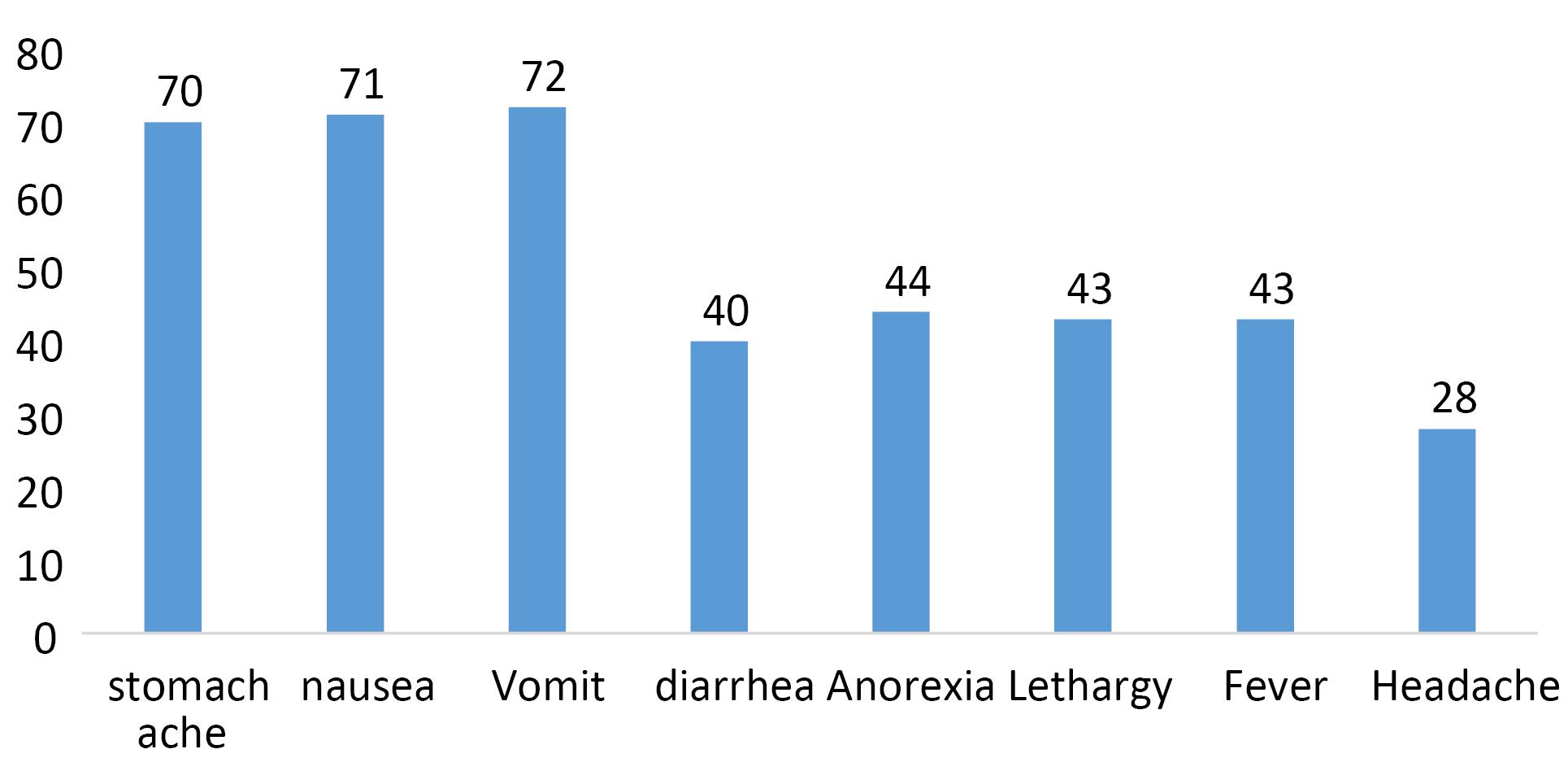
Figure 1.
Prevalence of Symptoms in Patients Examined in Mariyanaj Outbreak
.
Prevalence of Symptoms in Patients Examined in Mariyanaj Outbreak
Timely Reporting and Coordination
-
Defined a case as any Mariyanaj resident exhibiting symptoms from September 3, 2022.
-
Collected information from patients, drawing a daily chart (Figure 2).
-
Performed triage and rapid referral of cases.
-
Conducted interviews, obtaining medical histories and disease origin information.
-
Held a technical meeting with health and environment officials, experts, and disease management representatives.
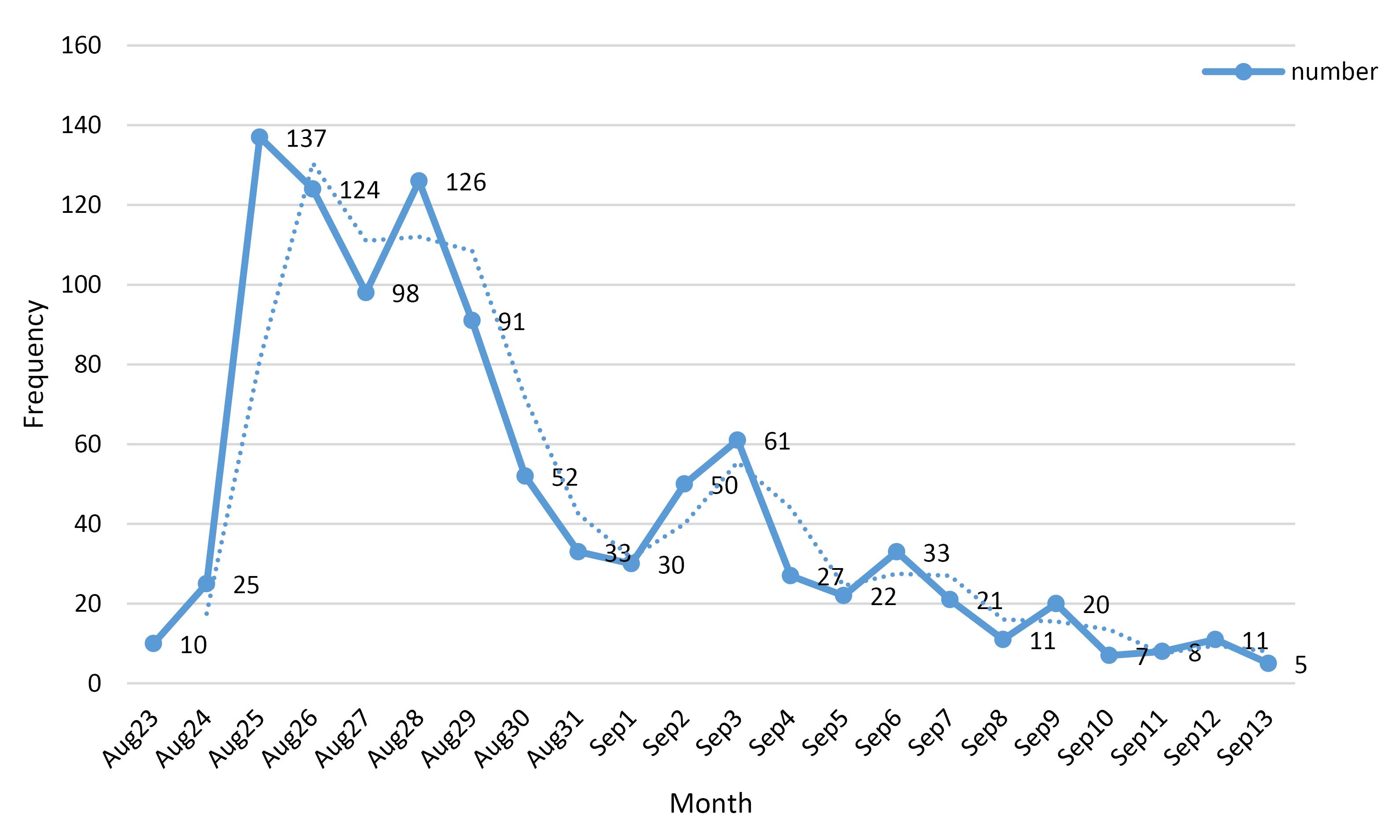
Figure 2.
Daily Trend of Cases from August 23 to September 13, 2022
.
Daily Trend of Cases from August 23 to September 13, 2022
Human and Food Sample Collection for Laboratory Testing
The following measures were taken:
Water Sampling
Patient’s water sources were examined, with a focus on sampling from drinking water tankers, household water sources of some patients, and a sports stadium. Personal wells used by patients during the water shortage crisis were also sampled. The water source and well of the Mariyanaj Comprehensive Health Services Center were sampled for the health of employees and visitors to identify any contaminants that could be responsible for the outbreak.
Obtaining Rectal Swabs
Coordination was made to obtain rectal swabs from symptomatic patients. Personnel were retrained in this regard to ensure the proper collection of samples.
Coronavirus Disease 2019 Sampling
COVID-19 sampling was conducted on a number of patients to investigate possible cases of COVID-19 with gastrointestinal symptoms.
Sampling for Symptom/Exposure
Samples were taken from some symptomatic patients (2 samples per person) and sent for examination to the laboratory of the Center for Disease Control.
Microbiological Culture of Water Samples
A full microbiological culture of water samples was conducted, including 3 samples from wells and 2 samples from the urban network. Results showed that 2 samples from the urban network were safe, while 3 samples from the wells were completely contaminated.
Culture of Water Samples
Full culture of water samples was conducted, including Staphylococcus, Streptococcus, Pseudomonas, total heterotrophic coliforms, and E. coli.
Virus Identification
Water samples were also taken for virus identification and sent to the virology laboratory.
Stool Sample Examination
Stool samples were sent to the Shahid Beheshti University of Medical Sciences for viral and bacterial examination.
Implementation of Control and Prevention Measures
The Completion of the Risk Assessment Form
A risk assessment form was completed to identify potential risk factors associated with the outbreak.
Individual Epidemiological Investigation
An individual epidemiological investigation form and a linear form were completed to gather information on affected individuals and draw a disease risk map. This information was summarized immediately to inform decision-making.
Field Visits
Representatives from the Disease Management Center conducted field visits to assess the situation on the ground, and the status of the chlorine in the water network of the city of Merianj was examined one week before the outbreak (Figure 3)
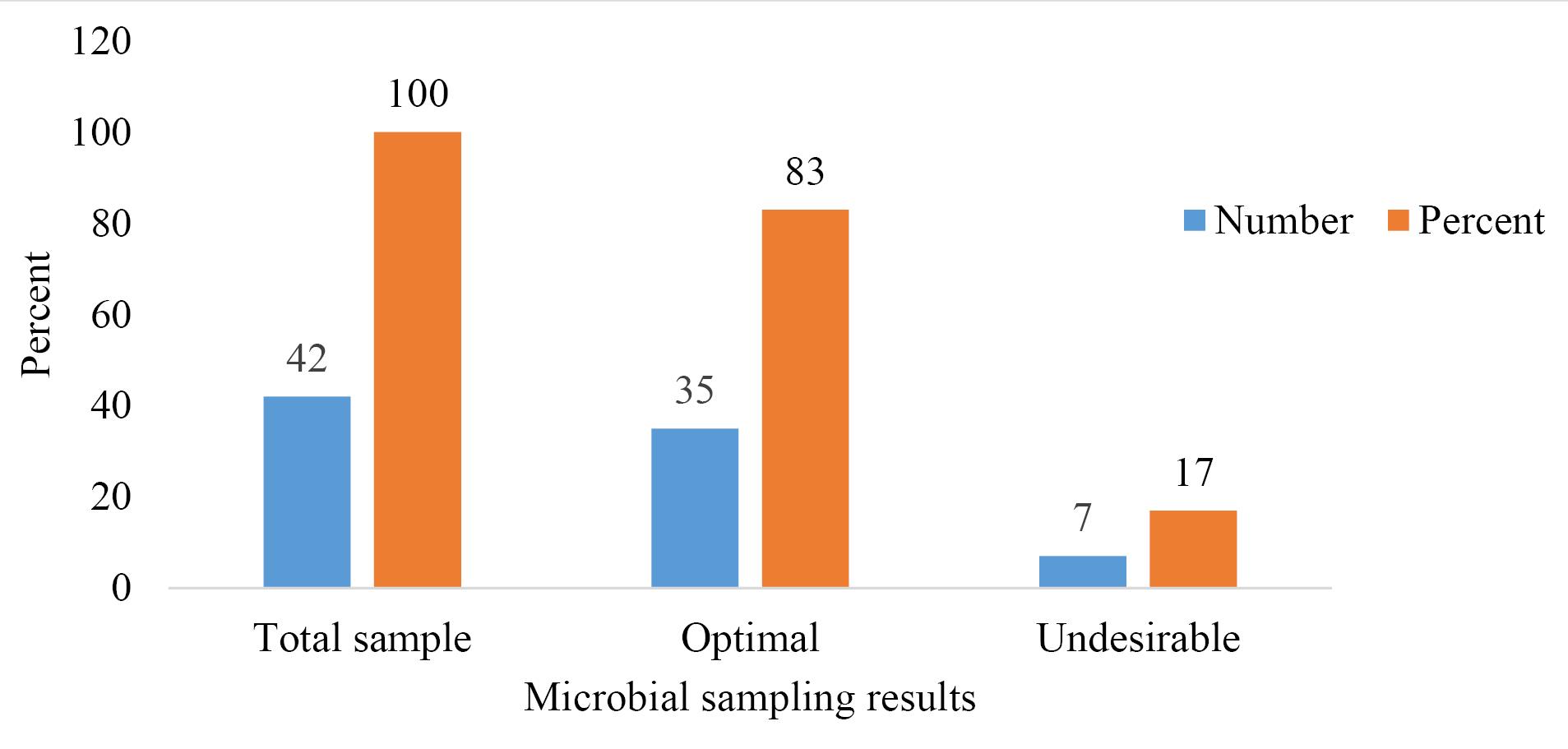
Figure 3.
The Number and Usefulness of Microbial Sampling Results of Meriyanaj’s Distribution Network (6 to 10 September 2022)
.
The Number and Usefulness of Microbial Sampling Results of Meriyanaj’s Distribution Network (6 to 10 September 2022)
Technical Evaluation
The technical team of the Health Department evaluated the situation to determine appropriate measures to control and prevent the spread of the disease.
Environmental Health Expert Teams
Monitoring and operational teams of environmental health experts were formed to investigate conditions in the region in the morning and afternoon.
Increased Chlorination
Daily chlorination in all hours of water supply in the network was increased to ensure the safety of drinking water.
Education on Water Sanitation
Universal education on water sanitation was provided, emphasizing the use of boiling or water purifiers. Chlorine powder and educational brochures on how to use it were also distributed.
Additional Medical Personnel
Coordination was made for the deployment of a second physician and one nurse or caregiver to provide additional medical support.
Drug Supply Coordination
Coordination was also made for the supply of drugs by the private sector pharmacy under contract and the supply of national quota drugs (serum and antibiotics) with the coordination of the Food and Drug Deputy from the Besat Hospital and the health center drugstore.
Rumor Management
Personnel were informed of rumor management techniques to create calm for the people in the area. The importance of water sanitation, not using household well water for drinking, boiling drinking water, using drinking water tankers for drinking water supply, and observing personal and food hygiene was emphasized. Chlorine and educational brochures were then distributed simultaneously.
Distribution of Mineral Water
Coordination was made with the Red Crescent to distribute free mineral water in the area under the discretion and order of the governor to ensure that people have access to safe drinking water.
Hospital Coordination
Coordination was made with Sina, Shahid Beheshti, and Army hospitals to report cases who were referred from Mariyanaj to those hospitals according to the definition.
Mapping of Disease Cases
Disease cases were mapped on the city map to identify areas of high risk and to inform future interventions.
Continuing Health Education
Health monitors at the Mariyanaj Comprehensive Health Center received continuing education on methods of water sanitation and hand washing to prevent the spread of the disease.
Organization Information Related to the Outbreak
During disease outbreaks, it is important to organize patient information to facilitate an effective response. The following steps describe how information was organized during a recent outbreak:
-
The first step was collecting data from various sources. A list of referrals was extracted from admissions records, including their national codes. Patients and physicians were interviewed to gather information on the referral process, prominent symptoms, affected age and gender groups, the involvement of family members, shared water and food sources, and hospitalized patients. The addresses and phone numbers of patients were extracted from the Sib system, and a histogram of cases during the outbreak period was drawn (Figure 4).
-
Next, new cases were identified and reported. Patients showing dangerous symptoms were immediately reported. Referrals were contacted to identify defined cases from the 11th to the 13th of September. Telephone interviews were then conducted by 7 health experts, and 4 expert teams were dispatched for field review. Another action was to map disease cases on a city map or mapping to find the spatial pattern of disease spread (Figure 5).
-
Patient information was then managed. The situation of previous referrals was followed up on, and a list of patients was maintained in all shifts. Forms were provided to private clinics, and case statistics were collected from hospitals such as Sina, Besat, and Army hospitals.
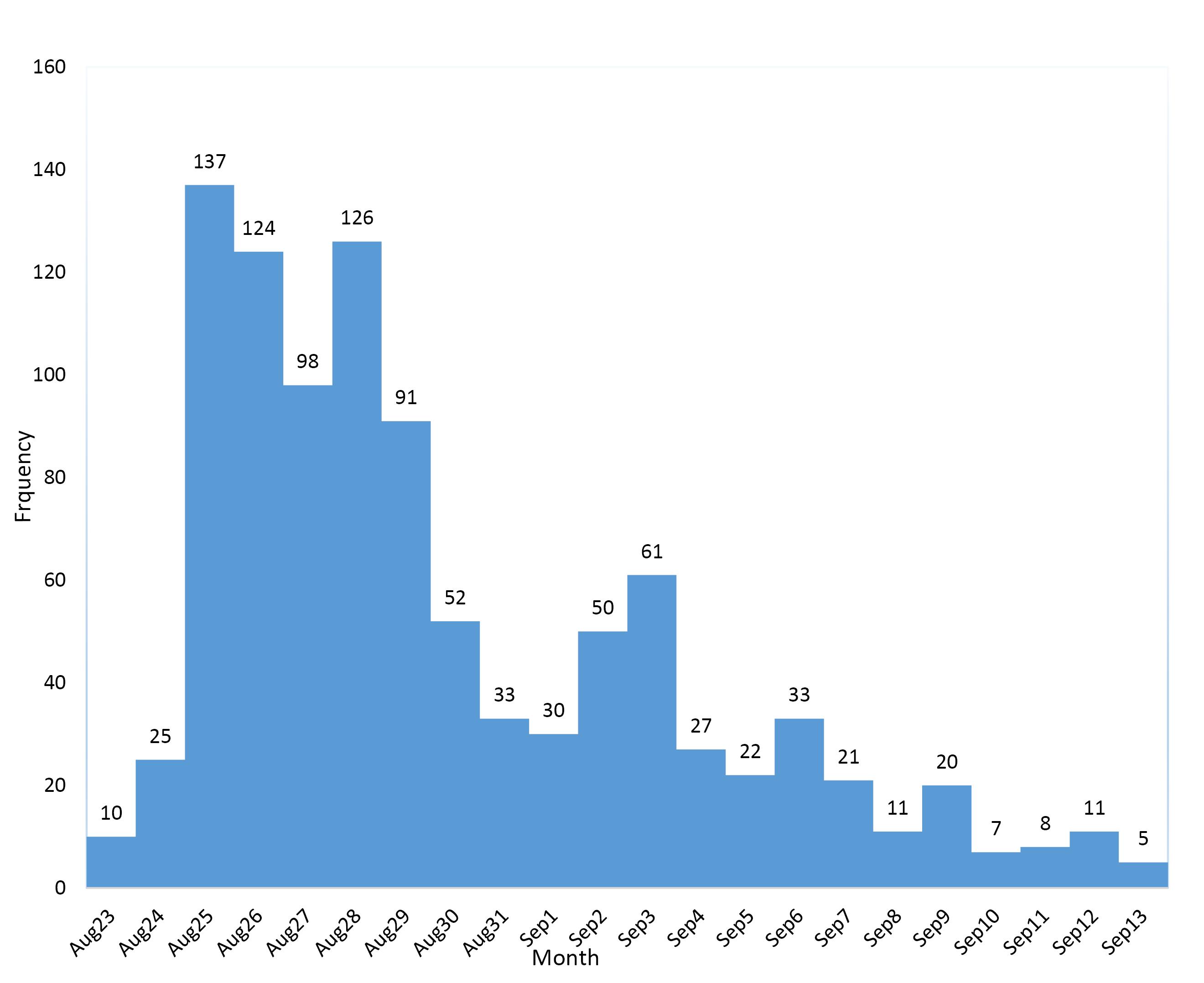
Figure 4.
Histogram of Cases of Gastroenteritis Outbreak in Mariyanaj from August 23 to September 13 in 2022
.
Histogram of Cases of Gastroenteritis Outbreak in Mariyanaj from August 23 to September 13 in 2022
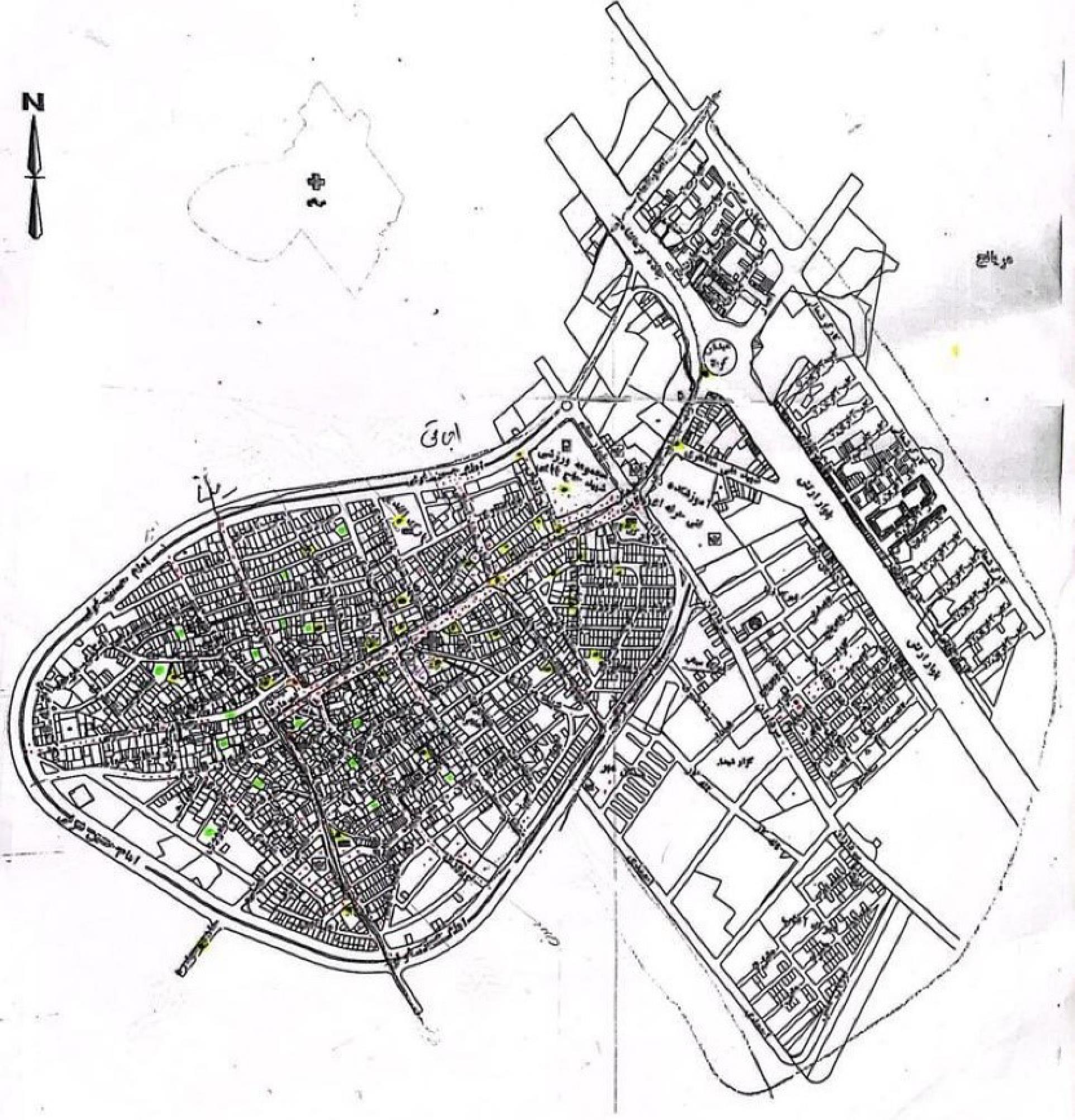
Figure 5.
Spot Map of Outbreak Cases in Mariyanaj
.
Spot Map of Outbreak Cases in Mariyanaj
Overall, an organized process was followed to systematically gather comprehensive data during the outbreak, including collecting information from multiple sources, identifying and reporting new cases, maintaining information on all patients, and involving relevant organizations. This approach ensured that all necessary information was gathered to inform outbreak response measures.
Developing a Hypothesis
Designing and Conducting an Epidemiological Study to Test a Hypothesis
This step involved completing a line list, conducting interviews, completing an epidemiological investigation form for patients, plotting the epidemiological curve of cases, designing a case-control study to investigate the cause, and implementing a case-control research project to investigate the causes and contributing factors.
Analyzing the Collected Data
Data were entered into SPSS-23 software, and the preliminary analysis of information was done by age, gender, and symptoms
Interpreting Findings and Drawing Conclusions
Presenting the Findings of the Outbreak Investigation
In conclusion, a comprehensive and systematic approach was employed, encompassing multiple steps to investigate and manage the outbreak effectively in Mariyanaj.
Results
To investigate this outbreak, the study included 919 individuals from Mariyanaj who developed symptoms of gastroenteritis. The epidemiological curve, displayed in Figure 1, exhibits a unimodal shape, indicating a common source for the outbreak. Figure 2 presents the epidemiological map, showcasing the distribution of cases and household water sources in Mariyanaj. The gender distribution among patients was 57.57% male and 43.43% female. The highest number of cases occurred in the age group of 10-14 years (19 individuals), followed by 16 individuals in the 5-9 years age group, and 10 individuals in the 15-19 years age group. The youngest patient was one-year old, and the oldest was 81 years old. Predominant symptoms included vomiting, nausea, and abdominal pain. Drinking water sources comprised 75.66% piped water, 30.26% well water, 5.4% tanker water, and 4.3% spring water.
Table 1 displays the results of the case-control study involving 133 individuals in the case group and 100 individuals in the control group. Both groups did not significantly differ in terms of age and gender (P > 0.05). Piped water showed the highest odds ratio (11.02) and a significant association with the outbreak (P = 0.001), while well water displayed a significant and inverse association (odds ratio: 0.4, P < 0.05). Furthermore, spring water and tanker water had no significant association with the outbreak (P > 0.05).
Table 1.
Reporting Odds Ratio for Sources of Drinking Water
|
Type of Drinking Water
|
Odds Ratio
|
Confidence Interval
|
Significance
|
| Pipe water usage |
11.7 |
5.64-21.724 |
0.001 |
| Well water usage |
0.4 |
0.22-0.72 |
0.002 |
| Spring water usage |
0.72 |
0.2-2.5 |
0.73 |
| Tanker water |
3.5 |
0.43-28.7 |
0.28 |
Table 2 presents the results of microbiological tests on patients, indicating that Shigella and E. coli have the highest rates of positivity.
Table 2.
Samples Examined in Some Patients in Mariyanaj Outbreak
|
Type of Sample
|
Positive Result
|
Negative
|
Total
|
|
Shigella
|
Norovirus
|
COVID-19 Positive
|
Nonpathogenic
Escherichia
coli
|
Campylobacter
|
Escherichia
coli
|
Giardia
|
| Swap rectal |
2 |
2 |
0 |
0 |
0 |
0 |
0 |
112 |
116 |
| PCR of COVID-19 |
0 |
0 |
6 |
0 |
0 |
0 |
0 |
11 |
17 |
| Stool exam |
3 |
1 |
0 |
2 |
1 |
18 |
1 |
35 |
57 |
Note PCR: Polymerase chain reaction.
Discussion
The research findings highlighted a noteworthy concentration of disease cases within the 10-14-year age group, shedding light on a distinctive vulnerability in this demographic. Notably, the results of the study revealed a higher prevalence of the disease in women, a deviation from the 2002 epidemic where no significant gender difference was noted (14). Examining parallels with the epidemic in Karaj, where non-piped water usage elevated the risk of infection by 5.1 times, the current investigation underscores that the consumption of municipal piped water escalates the disease risk by approximately 6 times, indicating its recognition as the primary outbreak source according to reports from water and wastewater company officials. Notably, recurrent disruptions in the urban water network, reported between September 20th and October 25th, were attributed to insufficient piped water supply, compounding the challenges posed by the outbreak (15).
Clinical manifestations underpinned by epidemiological studies and laboratory analyses confirming the presence of the Norwalk virus characterize patients with symptoms such as diarrhea and dehydration in the early stages, alongside abdominal pain and sporadic reports of headache or fever during the outbreak. These manifestations align with the pathogenesis of bacterial diseases, and E. coli as a potential contaminant, disseminating through diverse routes such as food or water, contributes to the complexity of the outbreak (16).
According to the WHO’s recommendations, a robust collection of 15 to 20 clinical samples during outbreaks is deemed imperative for effective epidemic investigation. A comparative note from a study conducted by Zeng Wei and colleagues in China revealed that despite the WHO guidelines, only 13 fecal samples were examined to confirm and investigate the outbreak, underlining the challenges associated with identifying the pathogen responsible for diarrhea outbreaks in developing countries. This accentuates the pivotal role of epidemiological research in identifying risk factors and implementing targeted control measures to address such outbreaks. Contaminated water-induced epidemics are particularly prevalent due to the proximity of sewage wells to water wells, as evidenced in previous studies (17,18).
A notable example was observed in Pardis city, where inadequate distance maintenance between the river and wells by the drinking water supplier, located on the riverbanks, led to water contamination. Additionally, the lack of proper distancing between these well water sources exacerbated the situation (19). In a study conducted in Kurdistan, a critical distinction emerged, indicating that 50% of floods resulted from water-related issues in households using chlorine-free drinking water, while the remaining 50% occurred in households employing chlorinated drinking water. The insufficiency of free chlorine and inadequacy of chlorine amounts were attributed to this significant disparity (20). A parallel revelation in the Kerman study displayed suboptimal microbial quality in drinking water and food sources in Iranshahr, emphasizing the need for heightened control measures at the source of distribution, rigorous purification processes, regular monitoring, and periodic inspections (21).
The primary cause of the outbreak in the study area was identified as water contamination, with a critical need for enhanced physical protection for wells supplying drinking water. Recommendations encompass public education on personal hygiene practices, modernization of the water and wastewater system, and preventive measures against repeated cuts and pressure drops in the city’s water supply to preclude future outbreaks (22). Despite these crucial insights, it is imperative to acknowledge potential limitations associated with the study. Information collection through telephone interviews may introduce reporting biases and inaccuracies compared to in-person interviews. The study predominantly focused on diagnosed patients within the health system, potentially overlooking undiagnosed or unreported cases in the community. Furthermore, the investigation occurred after the initial phase of the outbreak, limiting the establishment of clear temporal relationships between exposures and illnesses. Finally, conducting the study only in one city necessitates caution in generalizing findings to other communities facing similar outbreaks (23).
In sum, the study provides valuable insights, yet it is evident that larger and more rigorous investigations are needed to corroborate findings and establish evidence-based recommendations for outbreak response and prevention. In addition, the multifaceted nature of waterborne outbreaks demands a comprehensive and nuanced approach to effective public health management.
Conclusion
The current study meticulously investigated the outbreak in Mariyanaj through systematic adherence to WHO’s 10-step guidelines and unraveled a complex interplay of factors contributing to waterborne illness. The infiltration of microbial and viral agents into municipal piped water emerged as a critical factor. Recommendations for infrastructure repair, modernization of water and wastewater systems, and implementation of health education initiatives underscore the study’s holistic approach to outbreak prevention. These conclusions encapsulate not only the immediate response to the Mariyanaj outbreak but also offer a roadmap for bolstering public health measures and infrastructure resilience in the face of potential future challenges.
Acknowledgments
The authors extend their gratitude to the personnel of the Comprehensive Health Service Center of Hamadan and the Water and Sewage Department of Hamadan.
Authors’ Contribution
Conceptualization: Fateme Torkaman Asadi, Masoume Javaheri, Fahime Moeini.
Data curation: Masoume Javari, Karimi Hamid, Lida Rafati.
Formal analysis: Masoume Javaheri, Fahime Moeini, Salman Khazaei.
Funding acquisition: Fateme Torkaman Asadi.
Investigation: Fateme Torkaman Asadi, Masoume Javaheri, Fahime Moeini, Lida Rafati, Sepide Mikaeilinia, Mina Nikbakht.
Methodology: Masoume Javaheri, Fahime Moeini.
Project administration: Fateme Torkaman Asadi.
Software: Masoume Javaheri.
Supervision: Fateme Torkaman Asadi, Masoume Javaheri, Lida Rafati.
Validation: Salman Khazaei.
Visualization: Fateme Torkaman Asadi.
Writing–original draft: Fateme Torkaman Asadi, Masoume Javaheri, Fahime Moeini.
Writing–review & editing: Fateme Torkaman Asadi, Masoume Javaheri, Fahime Moeini.
Competing Interests
The authors declare that they have no conflict of interests.
Ethical Approval
The ethics committee of Hamadan University of Medical Sciences approved the study (IR.UMSHA.REC.1402.077).
Funding
This project has been supported by the Deputy of Health, Hamadan University of Medical Sciences, Hamadan, Iran.
References
- Shao D, Shi Z, Wei J, Ma Z. A brief review of foodborne zoonoses in China. Epidemiol Infect 2011; 139(10):1497-504. doi: 10.1017/s0950268811000872 [Crossref] [ Google Scholar]
- Ashbolt NJ. Microbial contamination of drinking water and disease outcomes in developing regions. Toxicology 2004; 198(1-3):229-38. doi: 10.1016/j.tox.2004.01.030 [Crossref] [ Google Scholar]
- Kindhauser MK. Communicable Diseases 2002: Global Defence Against the Infectious Disease Threat. Geneva; World Health Organization; 2003.
- Hinderliter J. From farm to table: how this little piggy was dragged through the market. USFL Rev 2005; 40:739-68. [ Google Scholar]
- Fosse J, Seegers H, Magras C. Foodborne zoonoses due to meat: a quantitative approach for a comparative risk assessment applied to pig slaughtering in Europe. Vet Res 2008; 39(1):1-16. doi: 10.1051/vetres:2007039 [Crossref] [ Google Scholar]
- Kasper MR, Lescano AG, Lucas C, Gilles D, Biese BJ, Stolovitz G. Diarrhea outbreak during US military training in El Salvador. PLoS One 2012; 7(7):e40404. doi: 10.1371/journal.pone.0040404 [Crossref] [ Google Scholar]
- WHO Western Pacific. Field Manual for Capacity Assessment of Health Facilities in Responding to Emergencies. WHO; 2006.
- Yang Z, Wu X, Li T, Li M, Zhong Y, Liu Y. Epidemiological survey and analysis on an outbreak of gastroenteritis due to water contamination. Biomed Environ Sci 2011; 24(3):275-83. doi: 10.3967/0895-3988.2011.03.011 [Crossref] [ Google Scholar]
- Masoumi Asl H, Gouya MM, Soltan-Dallal MM, Aghili N. Surveillance for foodborne disease outbreaks in Iran, 2006-2011. Med J Islam Repub Iran 2015; 29:285. [ Google Scholar]
- Organization WHO Prevention of foodborne disease: Five keys to safer food manual. World Health Organization Available from: http://www.who.int/foodsafety/publications/consumer/flyer_keys_en.pdf. Accessed 2013;5.
- Esterhameyan M, Masumi Asl H, Farsar AR, Shafeie T, Etemad K, Khorrami Z. Diarrhea outbreak associated with drinking water in Pardis city, Tehran 2014. Community Health 2018; 5(2):113-21. doi: 10.22037/ch.v5i2.17879.[Persian] [Crossref] [ Google Scholar]
- World Health Organization (WHO). Guidelines for the Control of Shigellosis, Including Epidemics Due to Shigella Dysenteriae Type 1. WHO; 2005.
- World Health Organization (WHO). Using Climate to Predict Infectious Disease Epidemics. WHO; 2005.
- Masoumi Asl H, Eshrati B, Hosseini M, Soroush M, Khadivi R, Bargian M, et al. Investigation of outbreaks of diarrhea in the Dah Cheshmeh village of Chaharmahal-Bakhtiari province, Farsan city, in July and August 2002. Journal of Infectious and Tropical Diseases 2003;10(28):11-4. [Persian].
- Barati H, Golmohmmadi A, Momeni I, Moradi G. A cholera outbreak investigation in Karaj district in 2008. Iran J Epidemiol 2010;6(3):28-34. [Persian].
- Dale K, Kirk M, Sinclair M, Hall R, Leder K. Reported waterborne outbreaks of gastrointestinal disease in Australia are predominantly associated with recreational exposure. Aust N Z J Public Health 2010; 34(5):527-30. doi: 10.1111/j.1753-6405.2010.00602.x [Crossref] [ Google Scholar]
- Zeng W, Jiang S, Liang X, Chen J, Peng Q, Li Z. Investigation of a community outbreak of diarrhea associated with drinking water in suburb of Chengdu, China. Open J Epidemiol 2015; 5(3):147-54. doi: 10.4236/ojepi.2015.53019 [Crossref] [ Google Scholar]
- Egoz N, Shmilovitz M, Kretzer B, Lucian M, Porat V, Raz R. An outbreak of Shigella sonnei infection due to contamination of a municipal water supply in northern Israel. J Infect 1991; 22(1):87-93. doi: 10.1016/0163-4453(91)91122-e [Crossref] [ Google Scholar]
- Ranjbar R, Rahbar M, Naghoni A, Farshad S, Davari A, Shahcheraghi F. A cholera outbreak associated with drinking contaminated well water. Arch Iran Med 2011; 14(5):339-40. [ Google Scholar]
- Ebrahimi SJ, Sadeghi S, Saghi MH, Faghih Solaimani P, Mostafavi F, Ebrahimzadeh L. Epidemiological study of the outbreak of waterborne and foodborne diseases in Kurdistan province. J Res Environ Health 2019; 5(3):239-48. doi: 10.22038/jreh.2019.38425.1280.[Persian] [Crossref] [ Google Scholar]
- Malkutian Mohammad, Yeghmayan Kamiyar, Jafari Mansooryan Hossein, Alizadeh Mustafa, & Jafari Madrak Mohammad. Investigating the prevalence and mortality rate of diseases transmitted by drinking water and food. Improving safety and preventing injuries 2015; 3(1): 15-24. [Persian].
- World Health Organization (WHO). Water, Sanitation and Hygiene for Disease Prevention and Control. 2019. Available from: https://www.who.int.
- Rogers SM, Miller HG, Turner CF. Effects of interview mode on bias in survey measurements of drug use: do respondent characteristics make a difference?. Subst Use Misuse 1998; 33(10):2179-200. doi: 10.3109/10826089809069820 [Crossref] [ Google Scholar]